Abstract
Background: The majority of subjects with a diagnosis of primary central nervous system lymphoma (PCSNL) have diffuse large B-cell lymphoma (DLBCL) as their histology. However, there are a sub-set of PCSNL patients who present with other histologies. This retrospective study was conducted to evaluate histological morphology, risk factors and clinical course in subjects with non-diffuse large B-cell primary CNS lymphoma.
Methods: We used the Mayo Clinic Lymphoma Database to search for patients with PCSNL during the time period from January 1995 to June 2018. One hundred and fifty nine patients met the criteria and underwent record review. One hundred and nine patients were excluded as they had PCSNL with DLBCL histology (N=47, 43%), secondary central nervous system lymphoma (N=56, 51%) and post-transplant lymphoproliferative disorders (PTLD) with DLBCL morphology (N=6, 5%). We identified fifty patients with PCSNL Non-DLBCL histology, by evaluating the biopsy reports. We abstracted clinical data and outcomes for these groups through medical chart review. Kaplan-Meier analysis was used to estimate survival.
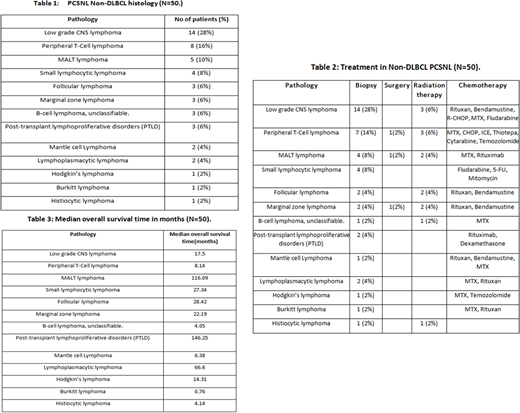
Results: The mean age of the study population was 70 ± 11.3 years and 66% were male. Of the 50 patients, the most common histology was low grade CNS lymphoma (N=14, 28%) while Hodgkin's lymphoma (N= 1, 2%), Burkitt's lymphoma (N= 1, 2%) and histiocytic lymphoma (N= 1, 2%) were the least common. The frequencies of other PCSNL Non-DLBCL histology are demonstrated in Table1. Most patients showed good ECOG performance status of 0-2 and four patients had ECOG performance status of grade 3 (N=4, 8%). Six of the patients were immunocompromised (N=6, 12%), PPD positive tuberculosis; corticosteroids and PTLD with DLBCL histology were the causes for the immunocompromised state. The location of the CNS lymphoma included brain (N=24, 50%); spinal cord (N=9, 18%); orbits (N=5, 10%); deep structures which included brainstem, cerebellum, cerebellopontine angle and cauda equina (N=5, 10%); leptomeninges (N=4, 8%) and neural involvement which included sciatic, peroneal and facial nerve (N=3, 6%). CSF examination revealed increased protein levels (N=10, 20%), malignant cells (N=11, 22%), negative cytology (N=14, 28%) and unknown or not done (N=15, 30%). Most patients presented with neurological symptoms such as seizures, peripheral neuropathy (numbness/weakness/tingling), headache, confusion & cognitive disturbances (memory changes), gait disturbances (difficulty with balance/ataxia), visual disturbances (blurry vision) and paraplegia, but none of them presented with B-cell symptoms such as fever, night sweats and weight loss. Treatment modalities included chemotherapy, radiation and surgery. Fourteen patients underwent radiation therapy (N=14, 28%); three of the patients had undergone surgery of which the patient with peripheral T-cell lymphoma had undergone a complete excision, the patient with marginal zone lymphoma had undergone debulking with subtotal craniotomy and the patient with MALT lymphoma had undergone resection with gamma knife. Table 2 demonstrates the various chemotherapy drugs used and the distribution of frequency of biopsy, radiation and surgical treatment in the different pathology of PCSNL Non-DLBCL.
The median overall survival period using Kaplan-Meier analysis showed that Burkitt's Lymphoma had the least median time survival of less than a month and PTLD had the highest median survival of 146.25 months (p=0.0017). Table 3 shows the median survival time for all the different pathology's of PCSNL Non-DLBCL.
Conclusion: This retrospective study reinforces the critical need for a histologic diagnosis when a patient is diagnosed with PCNSL. PCSNL is considered to be DLBCL but there are other histology's that could potentially be PCSNL and the treatment should be tailored to the individual patient's histology.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.