Abstract
Background:
Cytogenetic abnormalities occur in approximately a third of patients with primary myelofibrosis (PMF) and 5-20% of those with essential thrombocythemia (ET) or polycythemia vera (PV). Abnormal karyotype in PV and specific cytogenetic abnormalities in PMF have been shown to adversely affect survival (Leukemia. 2018;32:1189; Br J Haematol. 2017 Jun 9. doi: 10.1111/bjh.14798). In the current retrospective study, we considered 650 Mayo Clinic patients with myeloproliferative neoplasms (MPN), including ET, PV and PMF, with at least two documented bone marrow (BM) biopsies, in order to examine the incidence and pattern of changes in karyotype and their clinical correlates.
Methods:
Study patients were recruited from the Mayo Clinic, Rochester, MN, USA, based on documentation of at least two serial BM biopsies. Diagnoses were according to the 2016 World Health Organization criteria (Blood. 2016;127:2391). BM biopsy #1 referred to the baseline karyotype at time of initial diagnosis/referral and BM biopsy #2 to the first repeat BM biopsy after diagnosis. In addition to documenting the presence or absence of changes in karyotype, a notation was made regarding disease phase, at the time of the repeat biopsy, in order to allow accurate interpretation of the data and evaluation of survival impact.
Results:
650 patients with MPN, including 153 ET, 105 PV and 392 PMF, were included in the current study and had undergone at least two BM biopsies; 227 patients had three, 108 four, 48 five, 19 six, and 4 seven repeat BM biopsies during their clinical course.
Cytogenetic clonal evolution in patients with normal karyotype at baseline:
Baseline karyotype was normal in 466 (72%) patients, including 139 (91%) ET, 91 (87%) PV and 236 (60%) PMF. Clonal evolution, which constituted a change from "normal" to "abnormal" karyotype, was documented in 16 (12%) patients with ET, 22 (24%) with PV and 75 (33%) with PMF; the latter included favorable karyotype in 11% of the cases, unfavorable in 12% and very high risk (VHR) in 10%. 11 (69%) of the 16 documented cases of clonal evolution in ET, 10 (45%) of 22 in PV and 11 (15%) of 75 in PMF were accompanied by clinically evident progression to blast or fibrotic phase disease, at the time of the repeat BM biopsy.
Cytogenetic clonal evolution in patients with abnormal karyotype at baseline:
Baseline karyotype was abnormal in 187 (28%) patients, including 17 (9%) ET, 14 (13%) PV and 156 (40%) PMF. Additional changes in karyotype, during serial BM biopsies, were documented in 6 (35%) ET, 5 (36%) PV and 71 (46%) PMF patients. In PMF, the pattern of changes in karyotype included "favorable" to "favorable" in 7%; "favorable" to "unfavorable" in 13%; "favorable" to "VHR" in 5%; "unfavorable" to "unfavorable" in 13%; "unfavorable" to "VHR" in 3%; and "VHR" to "VHR" in 6%. All 11 (100%) patients with ET or PV who underwent clonal evolution displayed clinically overt disease transformation into leukemic or fibrotic phase disease, at the time of the repeat BM biopsy. Leukemic transformation at the time of the repeat BM biopsy was evident in 13 (18%) of the 71 PMF cases with clonal evolution.
Survival impact of cytogenetic clonal evolution without change in disease phase:
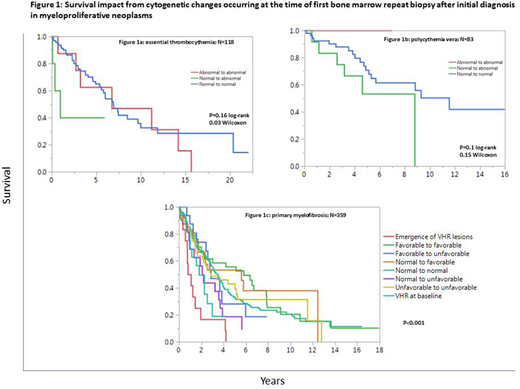
The survival impact of cytogenetic clonal evolution was examined under the following provisions: i) analysis was limited to events occurring at BM biopsy #2 with survival calculated from the date of BM biopsy #2; ii) patients with leukemic or fibrotic transformation at time of BM biopsy #2 were excluded from analysis; and iii) clonal evolution for the purposes of survival analysis constituted changes from "normal" to "abnormal", for ET and PV, while the type of changes were taken under consideration for PMF. Under these stipulations, clonal evolution appeared to affect survival in general, although statistical significance was apparent for only ET and PMF (Figures 1a, 1b and 1c).
Conclusions: Cytogenetic clonal evolution in ET and PV is infrequent, in the absence of clinically overt disease transformation, and is more likely to occur in PMF. Such events, when documented in chronic phase disease, appeared to predict shortened survival in all three MPNs, which was most apparent in ET and with emergence of VHR or unfavorable abnormalities in PMF. These observations warrant prospective studies that account for indication bias.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.