In this issue of Blood, Wagner and colleagues implicate Rip1 kinase (Ripk1)–mediated necroptosis in myelodysplastic syndrome (MDS)-like disease in mice and detect increased RIPK1 expression and mixed lineage kinase domain-like pseudokinase (MLKL) activation in human MDS samples.1
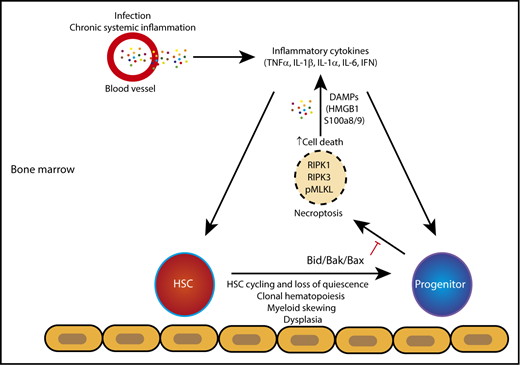
When apoptosis is disabled, mice develop MDS-like disease, characterized by increased Ripk1 expression and MLKL activation, features that are also observed in a subset of human MDS samples. HSC, hematopoietic stem cell; IFN, interferon; IL-1β, interleukin-1β.
When apoptosis is disabled, mice develop MDS-like disease, characterized by increased Ripk1 expression and MLKL activation, features that are also observed in a subset of human MDS samples. HSC, hematopoietic stem cell; IFN, interferon; IL-1β, interleukin-1β.
Cell death and an inflammatory gene signature have long been associated with the MDS hematologic disorder, which is characterized by abnormal differentiation, deficiency of mature blood cells, and predisposition to leukemia. Increased cell death in MDS has been attributed to apoptosis; however, many cell death methods fail to distinguish between apoptosis and other forms of inflammatory cell death such as necroptosis and pyroptosis. Whereas apoptosis is thought to be immunologically silent, necroptosis and pyroptosis result in membrane permeabilization and/or cation channel activation and the release of damage-associated molecular patterns (DAMPs). DAMPs are recognized by pattern recognition receptors (PRRs), and they stimulate cytokine and chemokine production, thereby inducing a feed-forward cycle of cell death and inflammation. DAMPs such as high mobility group box 1 (HMGB1) and the S100A8 and S100A9 alarmins are found in excess in MDS plasma2 where they bind Toll-like receptor 4 (TLR4) and other receptors to activate NF-κB and promote inflammation. In most cell types, necroptosis requires Mlkl and the kinase activities of Ripk1 and Ripk3. This form of inflammatory cell death can be activated downstream of death receptors (tumor necrosis factor [TNF], FAS, TNF-related apoptosis-inducing ligand [TRAIL]), PRRs such as TLR3 and TLR4, and type I or II interferon receptors. The serine/threonine kinase Ripk1 is a critical mediator of TNF signaling, which determines whether cell survival, apoptosis, or necroptosis ensues.
Wagner et al demonstrate that mice deficient in proapoptotic Bcl-2 family members Bax and Bak and the BH3-only family member Bid (designated triple knockout [TKO]) develop MDS-like features, including abnormal differentiation in the bone marrow, cytopenias, and leukemic progression. The Lin–Sca1+c-Kit+ population is increased and cycling in TKO mice, whereas myeloid progenitors are decreased. In the absence of apoptotic signals provided by Bak and Bax in double KO mice, Bid seems to coordinate the caspase-8–dependent cleavage of Ripk1 (and potentially Ripk3), thereby blocking necroptosis. Upon Bid loss in TKO mice, Ripk1 and Ripk3 are protected from cleavage by caspase-8. This results in increased levels of Ripk1 and Ripk3, Mlkl phosphorylation and oligomerization, and the appearance of cells with necrotic morphology in the bone marrow of TKO mice, suggesting that necroptosis underlies the progenitor cell loss (see figure) and bone marrow failure in these mice. Deregulated necroptosis in mouse hematopoietic cells induces systemic inflammation and depletes mouse hematopoietic stem and progenitor cells resulting in bone marrow failure. Inhibition of necroptosis or inflammatory signals in these mouse models restores hematopoiesis and significantly delays bone marrow failure.3,4
To demonstrate that Ripk1 mediates the progenitor cell loss and bone marrow failure in TKO mice, the authors reduce Ripk1 levels by deleting one Ripk1 allele, but they observe no significant change in the number of, or the proliferative status of hematopoietic progenitors. However, reduced Ripk1 expression is sufficient to restore red blood cell counts and hematocrits and reduce IL-1β and TNF-α expression in the bone marrow. Although these data suggest that necroptosis could be responsible, the increased cytokine/chemokine expression could reflect necroptotic independent functions of Ripk1 or Mlkl. The kinase activity of Ripk1 can influence cytokine and chemokine transcription,5 and Ripk1, Ripk3, and Mlkl can activate the nucleotide-binding domain and leucine-rich repeat pyrin domain containing 3 (NLRP3) inflammasome to produce IL-1β and IL-18 and/or stimulate pyroptosis.6,7 Consistent with this idea, NLRP3 inflammasome activation and pyroptosis have been observed in MDS patient samples and mouse models.8 To definitively demonstrate that necroptosis drives MDS pathogenesis will require genetic and pharmacologic approaches in multiple MDS mouse models and patient samples. Expression of kinase-inactive Ripk1 and analysis of MDS mouse models on Ripk3- and Mlkl-deficient backgrounds will provide genetic evidence to further implicate necroptosis in MDS. Similarly, human MDS studies focused on the effects of RIPK1 kinase or MLKL inhibitors in in vitro colony-forming assays and in vivo in MDS patient-derived xenografts should elucidate the inflammatory cell death pathways and mechanisms operative in human MDS.
Consistent with their mouse data, Wagner et al detect increased RIPK1 and phospho-MLKL expression in a small number of human MDS samples across disease subtypes. A prior history of infection or autoimmune disease increases the risk of MDS.9 Thus, infection or immune deregulation may induce proinflammatory cytokines such as TNF that, under conditions of caspase-8 inhibition, license cells to undergo necroptosis. Whether pyroptosis and/or necroptosis is engaged will likely reflect the specific cell types in the MDS bone marrow as well as the nature of the genetic mutations that make up the MDS clone(s). If necroptosis pathway activation holds up in larger studies of MDS patients, phospho-MLKL reactivity may serve as a useful biomarker for the disease and potentially for other inherited disorders that can lead to MDS. Perhaps most importantly, there is the possibility that RIPK1 kinase inhibitors, well tolerated in humans,10 may provide clinical benefit to MDS patients.
Conflict-of-interest disclosure: The authors declare no competing financial interests.