In this issue of Blood, Wang et al report correction of the bleeding phenotype in newborn and adult factor IX (FIX) knockout mice through in vivo gene editing mediated by clustered regularly interspaced short palindromic repeats/CRISPR associated protein 9 (CRISPR/Cas9).1 This technology involves a guide RNA that matches the target gene of interest and the endonuclease, Cas9, which introduces a double-stranded DNA-break enabling modifications to the genome.
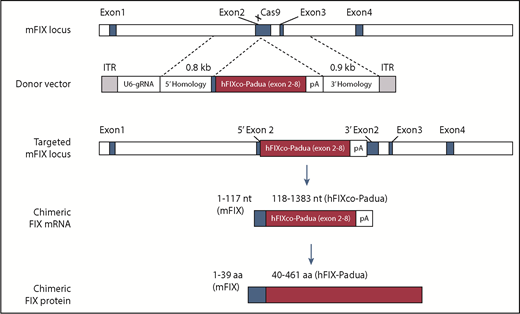
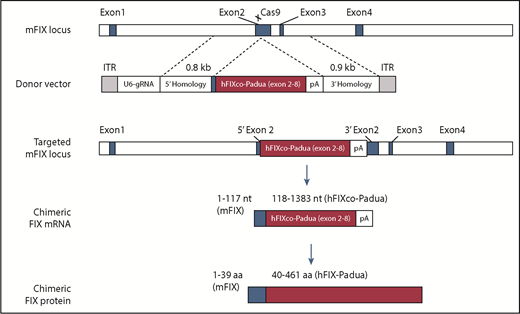
Schematic diagram shows the Cas9 target site located on exon 2 of the mouse FIX locus. Following homologous recombination with the AAV donor vector containing partial complementary DNA of codon-optimized hFIX-Padua, a chimeric FIX messenger RNA is transcribed from the modified FIX locus which is then translated to a chimeric FIX protein. See Figure 1 in the article by Wang et al that begins on page 2745.
Schematic diagram shows the Cas9 target site located on exon 2 of the mouse FIX locus. Following homologous recombination with the AAV donor vector containing partial complementary DNA of codon-optimized hFIX-Padua, a chimeric FIX messenger RNA is transcribed from the modified FIX locus which is then translated to a chimeric FIX protein. See Figure 1 in the article by Wang et al that begins on page 2745.
Hemophilia B (HemB), a serious hemostatic disorder resulting from mutations in the FIX gene, is an attractive target for gene therapy. Clinical trials using adeno-associated viral (AAV) vectors, without any genome editing, have shown successful amelioration of the severe bleeding phenotype of adults with severe HemB, eliminating the need for prophylactic FIX replacement therapy. The transgene assumes a stable episomal configuration capable of RNA transcription and subsequent protein translation. The durability of this treatment is evidenced by stable FIX expression for the past 10 years.2 However, these long-lasting therapeutic effects may not be reproducible in pediatric patients, those with the most to gain from effective bleed control, because of high hepatocyte cellular turnover, resultant dilution of transduced cells, and eventual loss of transgene expression.3 In addition, participants in these trials receiving high vector doses have exhibited cytotoxic T-cell responses against the viral capsid that can lead to loss of transgene expression that is not reliably prevented with transient treatment with systemic corticosteroids.4 Although AAV is considered a primarily nonintegrating vector, an unknown but small amount of the cassette integrates into the genome, with a potential risk of genotoxicity at insertion sites.
Gene correction approaches based on nuclease-driven homology-directed repair (HDR) are emerging as attractive alternatives to nongenome editing gene therapies for monogenic diseases such as HemB, with the advantage of ameliorating the risk from integration events. These techniques include zinc-finger nuclease (ZFN)-based HDR,5,6 transcription activator-like effector nuclease-based HDR,7 and the CRISPR/Cas9 gene editing technology. Among these, the CRISPR/Cas9 technology appears to be the most versatile, with several recent reports claiming correction of HemB in murine and canine models.3,7-9
Wang et al use a dual AAV8 vector system that includes a donor vector that contains a promoterless, codon-optimized, partial human FIX complementary DNA (exons 2 to 8) carrying the hyperactive FIX Padua mutation and a single guide RNA vector to target exon 2 of murine FIX. Targeting this region of the FIX gene is likely to have the broadest applicability because ∼90% to 95% of HemB mutations are 3′ to exon 1. They have established stable expression of FIX over an 8-month period in newborn and adult FIX-knockout mice following a single injection of the dual AAV gene-targeting vectors. The approach is similar to that described previously by Li et al5 ; however, Wang et al have used the hyperactive Padua variant, which increases the FIX-specific activity by up to 10-fold. They further demonstrate that the treated mice not only survived a partial hepatectomy 8 weeks after injection of the vector, but their FIX levels persisted for an additional 24 weeks posthepatectomy, indicative of stable genomic targeting. This strategy is unlikely to be handicapped by issues such as loss of the transgene with hepatocyte turnover that would occur with AAV vector–mediated episomal transgene therapy. Furthermore, using a single injection of a dual AAV8 vector system seems to be superior to other genome editing strategies such as those employing ZFNs that require the much less efficient, cotransduction of 3 vectors in the same cell (www.clinicaltrials.org, NCT02695160) (see figure).
Despite the exciting observations that Wang et al have reported, there are still some unresolved issues that require careful attention to extend this approach to the clinical setting. The high vector dose used in this approach raises concerns about AAV-related toxicity, including immune responses to the viral capsid. Will the dual vector system prove equally efficient in humans? Besides, the strategy of targeting the FIX exon 2 will not serve HemB patients with mutations within the FIX promoter region or the signal peptide. The possibility of off-target edits is particularly relevant and needs careful assessment not just by in silico techniques, but also by experimental analyses described recently.10
“To be or not to be – gene edited?” has been an ethically challenging question for the scientific community. Although CRISPR-based germline editing within human embryos is bound to remain controversial until such time that the ethical boundaries and safety issues regarding use of genome editing are clearly delineated, its therapeutic applications predominantly directed at somatic cells has generated considerable investment within biomedical research.
The first US clinical trial of CRISPR in somatic cells is now under way at the University of Pennsylvania with 2 patients, 1 with multiple myeloma and the other with synovial sarcoma (www.clinicaltrials.org, NCT03399448). Although this is the first of its kind in the United States, human trials with CRISPR have been in progress since 2016 in China in 12 patients with metastatic non-small cell lung cancer. Preliminary results indicate that the therapy is safe thus far (www.clinicaltrials.org, NCT02793856), although there is still a risk that editing could introduce a transformed clone of cells with malignant potential.
Despite the tremendous promise, there are still technical limitations challenging gene editing progress toward the clinic, especially in hemophilia. This disorder has benefitted considerably from biomedical innovations that have brought multiple novel therapeutics to the clinic, some of which have dramatically reduced the burden of prophylactic therapy while providing high efficacy. Nevertheless, the possibility of a “one and done” approach to produce durable, steady-state hemostasis, virtually eliminating regular prophylactic replacement and thereby resulting in annualized savings, has been a decades-long aspiration for this community. To supplant current therapies with gene therapy in general, and gene editing in particular, careful consideration needs to be given to identifying and eliminating possible off-target edits, choosing an appropriate and safe vehicle for in vivo delivery without any associated toxicity, and assessment of the risk-to-benefit ratio for each individual.
Conflict-of-interest disclosure: The authors declare no competing financial interests.