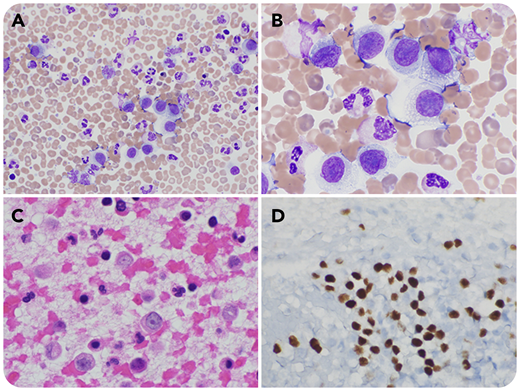
A 46-year-old woman was admitted to the hospital after developing seizure-like activity and altered mental status while receiving chemotherapy for metastatic melanoma. She originally was found to have superficial spreading melanoma of the left lateral calf, Clark level 4, which subsequently metastasized to the brain and lymph nodes. During the admission workup, a routine complete blood count demonstrated leukocytosis (22.3 × 10⁹/L) with a manual differential identifying 7% “other cells.” The peripheral smear illustrated a population of large-sized cells with abundant cytoplasm, irregular nuclei, and prominent nucleoli (panel A, original magnification ×40, Wright-Giemsa stain; panel B, original magnification ×100, Wright-Giemsa stain). A formalin-fixed paraffin-embedded block was made from a buffy coat of the patient’s blood. A hematoxylin and eosin stain (H&E) of the buffy-coat clot showed a population of large cells with abundant eosinophilic cytoplasm, irregular nuclei, and prominent red nucleoli (panel C, original magnification ×40, H&E stain). Immunohistochemically, the cells were positive for S100 and SOX-10 (panel D, original magnification ×20, SOX-10 stain).
This represents a rare example of peripherally circulating melanoma cells, and one of the few cases demonstrated by immunohistochemical staining. Following these findings, our patient elected to discontinue treatment and pursue palliative care.
A 46-year-old woman was admitted to the hospital after developing seizure-like activity and altered mental status while receiving chemotherapy for metastatic melanoma. She originally was found to have superficial spreading melanoma of the left lateral calf, Clark level 4, which subsequently metastasized to the brain and lymph nodes. During the admission workup, a routine complete blood count demonstrated leukocytosis (22.3 × 10⁹/L) with a manual differential identifying 7% “other cells.” The peripheral smear illustrated a population of large-sized cells with abundant cytoplasm, irregular nuclei, and prominent nucleoli (panel A, original magnification ×40, Wright-Giemsa stain; panel B, original magnification ×100, Wright-Giemsa stain). A formalin-fixed paraffin-embedded block was made from a buffy coat of the patient’s blood. A hematoxylin and eosin stain (H&E) of the buffy-coat clot showed a population of large cells with abundant eosinophilic cytoplasm, irregular nuclei, and prominent red nucleoli (panel C, original magnification ×40, H&E stain). Immunohistochemically, the cells were positive for S100 and SOX-10 (panel D, original magnification ×20, SOX-10 stain).
This represents a rare example of peripherally circulating melanoma cells, and one of the few cases demonstrated by immunohistochemical staining. Following these findings, our patient elected to discontinue treatment and pursue palliative care.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit http://imagebank.hematology.org.