Key Points
iTTP in older patients has atypical clinical features delaying diagnosis; 1-month and 1-year mortality rates are higher.
A history of iTTP in older patients negatively impacts the life expectancy in survivors.
Abstract
Older age is associated with increased mortality in immune thrombotic thrombocytopenic purpura (iTTP). Yet, data are scarce regarding iTTP occurring among older patients. To assess clinical features and long-term impact of iTTP on mortality in older patients (>60 years old), characteristics and prognoses of adult iTTP patients enrolled in the French Reference Center for Thrombotic Microangiopathies registry between 2000 and 2016 were described according to age (<60 years old or ≥60 years old). Long-term mortality of iTTP older survivors was compared with that of non-iTTP geriatric subjects. Comparing, respectively, older iTTP patients (N = 71) with younger patients (N = 340), time from hospital admission to diagnosis was longer (P < .0001); at diagnosis, delirium (P = .034), behavior impairment (P = .045), renal involvement (P < .0001), and elevated troponin level (P = .025) were more important whereas cytopenias were less profound (platelet count, 22 × 103/mm3 [9-57] vs 13 × 103/mm3 [9-21], respectively [P = .002]; hemoglobin level, 9 g/dL [8-11] vs 8 g/dL [7-10], respectively [P = .0007]). Short- and mid-term mortalities were higher (P < .0001) and increased for every 10 years of age range. Age ≥60 years, cardiac involvement, increased plasma creatinine level, and total plasma exchange volume were independently associated with 1-month mortality. Compared with a non-iTTP geriatric population, older survivors showed an increased long-term mortality (hazard ratio = 3.44; P < .001). In conclusion, older iTTP patients have atypical neurological presentation delaying the diagnosis. Age negatively impacts short-term but also long-term mortality.
Introduction
Immune thrombotic thrombocytopenic purpura (iTTP) is a thrombotic microangiopathy (TMA) characterized by the association of microangiopathic hemolytic anemia, profound thrombocytopenia, and organ impairment.1 The diagnosis is confirmed by the identification of a severe deficiency in ADAMTS-13, the von Willebrand factor–cleaving protease, and presence of anti-ADAMTS-13 antibodies.2 ADAMTS‐13 deficiency triggers the adhesion and aggregation of platelets to ultra-large von Willebrand multimers in capillaries and arterioles, resulting in microvascular thrombosis responsible for organ failure.3 iTTP is lethal in the absence of treatment. Older age, neurological and cardiac involvements, and lactate dehydrogenase (LDH) levels have been identified as risk factors for mortality.4,5 Nevertheless, prognosis has been dramatically improved combining daily plasma exchange, corticosteroids, and B-cell depletion with the monoclonal antibody rituximab,6 with current survival rates of >85%. Moreover, the recently available anti–von Willebrand factor nanobody caplacizumab could still improve survival.7,8 However, early mortality in iTTP was found systematically higher among older patients.4,9,10 Surprisingly, although the proportion of older patients in iTTP registries is significant (17% of patients are >60 years old and 13% are >70 years old) and may increase in the future as a result of a more systematic long-term follow-up of these older patients,11 the characteristics of iTTP among older patients have been poorly investigated so far.4 A history of iTTP was reported to impair long-term survival in younger patients and this long-term effect could be even more pronounced among older patients.12 It is, therefore, crucial to better understand the characteristics of iTTP among older patients, including short-term and long-term outcomes, to improve its prognosis in this population.
Methods
Patients and data collection
All data from iTTP patients referred to the French Reference Center for Thrombotic Microangiopathies from 2000 to 2016 were analyzed. For the present study, we only considered patients with complete data for clinical presentation, treatment, and long-term follow-up. iTTP patients were separated according to their age (under 60 years of age, or 60 years of age or older). As in previous studies, TTP diagnosis criteria were as follows13,14 : (1) the presence of Coombs-negative microangiopathic hemolytic anemia or microangiopathic hemolysis, (2) acute peripheral thrombocytopenia (<150 × 103/mm3) with the absence of any other identifiable cause of thrombocytopenia and microangiopathic hemolytic anemia (severe disseminated intravascular coagulopathy, malignant hypertension), and (3) severe acquired ADAMTS-13 deficiency (<10% of activity) with anti–ADAMTS-13 antibodies ≥15 U/mL. Cerebral involvement was considered in case of presence of headaches, delirium, seizures, focal deficiency, vigilance, and behavioral impairment. Cardiac involvement included novel sign of heart failure, chest pain, and, when available, electrocardiogram abnormality and increased troponin level. ADAMTS-13 activity and anti–ADAMTS-13 antibodies and other biological parameters were assessed as previously reported.1 Collected data included any past history of cardiovascular risk factors (dyslipidemia, hypertension, diabetes mellitus, and previous or current tobacco use), a preexisting history of ischemic heart disease, ischemic stroke, chronic kidney disease (according to Kidney Disease Improving Global Outcomes [KDIGO] classification), cognitive impairment, institutionalization and use of antihypertensive treatment, and antiplatelet or vitamin K antagonist. iTTP-associated comorbidities such as cancer, autoimmune disease, drugs, or infection were collected.
Treatment and outcomes
Delays from admission to diagnosis and from diagnosis to treatment and iTTP management were analyzed. Adverse events related to iTTP treatment were reported. Assessment of response to treatment was performed as previously described and in accordance with international recommendations15 : a complete response was defined as full resolution of any clinical manifestations and platelet count recovery (>150 × 103/mm3) for at least 2 days. Refractoriness was defined as the absence of platelet count doubling after 4 full days of standard intensive treatment with persistently elevated LDH levels. Exacerbation was defined by initial treatment response but reappearance of clinical manifestations and/or thrombocytopenia (<100 × 103/mm3 for at least 2 days) before durable remission (complete response with no further thrombocytopenia or clinical worsening for >30 consecutive days from the first day of platelet count recovery including the time on maintenance plasma exchange). Relapse was the reappearance of clinical features of iTTP (thrombocytopenia [<100 × 103/mm3 for at least 2 days], associated or not with neurologic manifestations) with no other identifiable cause after durable remission had been achieved.5 Survival status at 1 year (mid-term) and at the time of completion of the study (long-term) were completed by registry office and phone calls to general practitioners.
Ethics
The study has been approved by the French Data Protection Authority (Commission Nationale Informatique et Libertés [CNIL]; authorization no. DR-2012-158).
The Three-City Study
To evaluate the impact of iTTP on long-term mortality in older patients, we compared the survival rate of older patients from our study (iTTP patients) still alive at 1 month with that of older non-iTTP subjects, all participants of a population-based cohort on aging and dementia, the Three City (3C) Study. The protocol has been detailed previously.16 The present sample included 1755 community dwelling adults, initially aged 65 years, living in Bordeaux (N = 2104) and followed-up every 2 to 3 years over 17 years since 1999. The 1755 analyzed patients where those who completed all clinical data at the first visit after inclusion. Vital status of all participants was ascertained from family, general practitioners, or native city council until 17 years after the baseline visit. This study was conducted according to the guidelines laid down in the Declaration of Helsinki.
Statistics
Quantitative variables were summarized as median [interquartile range] and compared by use of the Mann-Whitney Wilcoxon rank-sum test. Categorical data were summarized as count (percentage) and compared by use of the χ2 or Fisher tests. To explore the effect of age, all analyses distinguished 2 age groups: patients 60 years of age and older vs patients under 60 years of age. Risk factors for short- and mid-term mortalities were investigated by logistic regression. First, a univariate analysis was performed. Only variables with a P < .20 and with <20% of missing data were included in the multivariable analysis.
We then evaluated the impact of iTTP on long-term survival in older patients compared with a control aging population. Data were available for 38 of 45 older iTTP survivors (mean length of follow-up after iTTP diagnosis, 1678 days [±1257]; median, 1682 [interquartile range (IQR), 1728]). A first comparison on clinical characteristics was done between the 2 populations. Then, survival analyses have been conducted using first Kaplan-Meier methods with pointwise limits, then a Cox proportional hazards model. We applied a backward stepwise selection controlled for sex, age, tobacco consumption, diabetes mellitus, stroke, cancer, hypertension, ischemic coronary disease, dementia, chronic kidney disease, and chronic obstructive pulmonary disease (COPD). Statistical analyses were assessed by R 3.5.1 statistical software (R Foundation for Statistical Computing, Vienna, Austria).
Results
Population characteristics and iTTP presentation
A total of 770 adult patients with features of TMA and a severe ADAMTS13 deficiency were included in our registry between October 2000 and December 2016. Among these patients, 27 had an alternative diagnosis (mostly severe sepsis/septic shock) and 22 had a congenital form of the disease. Three hundred ten others had insufficient data regarding clinical presentation and management, and/or incomplete follow-up, or were lost to follow-up, leaving 411 patients, of whom 71 (17%) were ≥60 years old (Figure 1). To ascertain that our cohort of studied patients was fully representative of the whole iTTP population, we verified that the main initial characteristics remained unchanged with and without the nonincluded patients. Among the 310 nonincluded patients, data about initial characteristics were available for 173 (136 were younger than 60 years of age, and 37 were 60 years of age or older). We found that comparisons were similar when those patients were included in the analysis (supplemental Table 1, available on the Blood Web site). As expected, older patients presented more comorbidities as suggested by the Charlson score, mostly cardiovascular diseases and cancer; hence, they were receiving more often antihypertensive treatment, antiplatelet therapy, and vitamin K antagonists. Patients with an initial episode and those with relapses were in comparable proportions between older and younger patients (Table 1). Most patients lived at home.
Older iTTP patients more frequently presented delirium with behavioral disturbance compared with younger ones, whereas headaches and abdominal pain were associated with younger age. Acute renal and cardiac injuries were more prevalent in older patients with increased plasma creatinine and troponin levels, respectively. Moreover, thrombocytopenia and anemia were more pronounced in younger patients. Interestingly, when we applied the French score on both groups of patients,14 we found that among patients most likely to have a severe ADAMTS-13 deficiency on diagnosis (platelets, ≤30 × 103/mm3; serum creatinine, ≤2.25 mg/dL), 80% of patients of the younger group had a confirmed severe ADAMTS-13 deficiency, vs only 61% in the older group (P < .0001) (supplemental Table 2), highlighting that diagnosing iTTP among older patients on the basis of clinical scores can be more challenging.
Although a history of cancer was more frequently observed in older iTTP patients compared with younger ones, autoimmune diseases were less often present. Other iTTP-associated diseases were comparable between groups.
iTTP treatment and morbimortality
Time from hospital admission to diagnosis was longer for older than for younger iTTP patients (3 days vs 1 day, respectively; P: .0001), consistent with a delayed diagnosis in the elderly, whereas time from diagnosis to treatment initiation was similar. To tentatively address the reasons leading to a delayed diagnostic, we focused more on the diagnostic context in older patients from individual clinical records when available (N = 67). In 17 patients, no obvious diagnostic delay could be seen. In the remaining patients with a possible diagnostic delay, however, iTTP diagnosis was preceded by neurological manifestations (26 cases) including malaise with or without loss of consciousness (3 cases), transient ischemic stroke leading typically to focal deficiency and/or aphasia (14 cases), behavior abnormalities/delirium/vigilance impairment (6 cases), seizure (2 cases), and dizziness (1 case). One additional patient had a myocardial infarction. In 16 other patients, we found that iTTP diagnosis was preceded by an infectious-like process, especially diarrhea (7 cases).
Treatment was comparable between age groups, including the proportion of patients treated with rituximab. Moreover, the increasing use of rituximab through the inclusion period was comparable between both groups as the slopes of the curves representing the percentage of patients treated by rituximab year per year were comparable between earlier and later years (supplemental Figure 1). Nevertheless, when treated, older patients received on average 1 fewer rituximab infusion than younger patients (Table 2).
Lethal and nonlethal catheter-related adverse events were similar between age groups. However, older patients more frequently experienced catheter self-removals or physical restraint prescription in order to avoid these removals (Table 2).
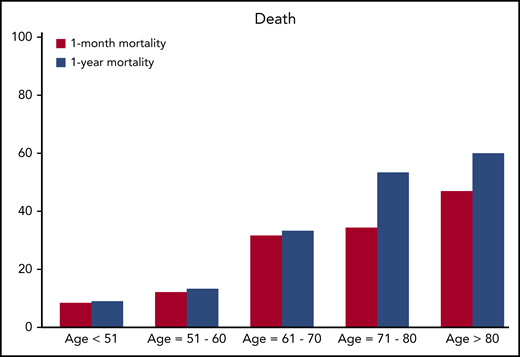
Short-term and mid-term mortality rates were increased in older patients (Table 3) and 1-month mortality increased for every 10-year range of age (Figure 2). Short-term mortality was mostly due to cardiac and neurological events. In fact, cause of death was tentatively identified for 18 of 26 patients: 8 of them died of a cardiac event (4 cardiogenic shocks, 3 cardiac arrests, and 1 ventricular arrhythmia), 8 died of a neurological event (6 ischemic strokes and 2 intracranial hemorrhages), 1 from mesenteric ischemia, and 1 from septic shock. Regarding mid-term mortality, cause of death was identified for 5 of 8 patients: stroke and septic shocks secondary to pneumonia (2 cases each) and cancer (1 case). Older iTTP survivors were also less likely to stay at home after discharge than younger survivors. No difference was found comparing older iTTP 1-month survivors to younger ones regarding relapse rate (3 of 30 [10%] vs 68 of 308 [22%], respectively; P: .23) and time to relapse (610 days [410; 695] vs 845 days [373; 1338], respectively; P: .37) (Table 3).
Assessed by multivariate analysis, age older than 60 years (odds ratio [OR], 33.3; IC95, 7.14-1000), cardiac involvement (OR, 5.88; 95% confidence interval (CI), 1.11-33.3), and increased plasma creatinine level (per +10 µmol/L; OR, 1.04; IC95, 1.01-1.1) were independently associated with 1-month mortality in the whole iTTP population. Plasma exchange volume was independently associated with a lower 1-month mortality (per +100 mL/kg; OR, 0.81; IC95, 0.60-0.98) (Table 4). Regarding mid-term mortality among older iTTP patients, we found cardiac involvement to be an independent risk factor (OR, 6.67; 97.5% CI, 1.89-25; P: .004).
Long-term mortality among older patients after durable iTTP remission compared with control non-iTTP elders (3C study)
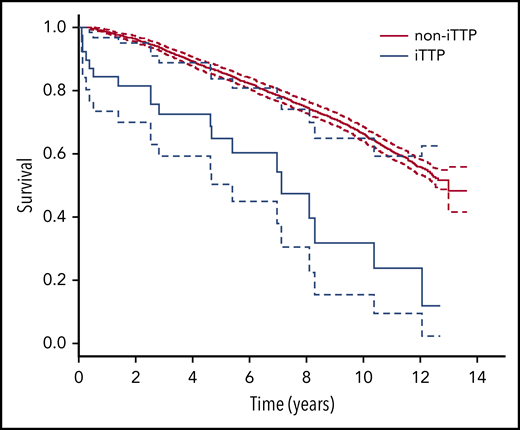
Long-term mortality data were available for 38 of 45 older iTTP survivors (mean length of follow-up after iTTP diagnosis, 1678 days (±1257); median, 1682 [IQR, 1728]) and were compared with those of 1755 non-iTTP geriatric cohort participants (Three-City Study cohort). Older iTTP 1-month survivors had more cardiovascular comorbidities and COPD (supplemental Table 3). They exhibited a lower long-term survival rate (Figure 3). A history of iTTP remained an independent risk factor for death (HR, 3.44; 95% CI [2.02; 5.87]) even after controlling for age, sex, cardiovascular risk factors and events, COPD, chronic kidney disease, and dementia (Table 5).
Comparison of long-term survival rates according to time between older iTTP survivors and the Three-City Study population (Kaplan-Meier curves). Log-rank: full line, survival rate; dashed line, 95% CI. iTTP, 1-month iTTP survivors ≥60 years old; Non-iTTP, population of the geriatric Three-City Study who do not have iTTP.
Comparison of long-term survival rates according to time between older iTTP survivors and the Three-City Study population (Kaplan-Meier curves). Log-rank: full line, survival rate; dashed line, 95% CI. iTTP, 1-month iTTP survivors ≥60 years old; Non-iTTP, population of the geriatric Three-City Study who do not have iTTP.
Discussion
Our data highlight the frequent atypical presentation of iTTP among older patients with more organ involvement, delirium, and behavioral abnormalities, and less pronounced cytopenias than younger patients, which may have contributed to a later diagnosis. Alternatively, organ damage in older patients following microthrombi formation may occur earlier than in younger patients, accounting for earlier clinical manifestations with older age; in younger patients, conversely, organs may be more tolerant to microthrombi and ischemia, leaving cytopenias to get worse. As a consequence of these features, we provide evidence that the diagnosis of iTTP based on clinical scores aimed at predicting a severe ADAMTS-13 deficiency14,17 may be less reliable among older patients. Not only delirium and acute behavioral abnormalities but also ischemic stroke are very common reasons to admit an older patient to hospital as they are not specific to a disease and are less alarming than in younger patients. This presentation could explain the delayed iTTP diagnosis in this age group. In this context, the presence of a thrombocytopenia with anemia should alert physicians to this possible rare diagnosis. Treatment between the 2 age groups was comparable; however, maintaining a catheter was more difficult in the older group because of poor venous access and behavioral disturbance frequently leading to catheter self-removals.
Short-term (1-month) and mid-term (1-year) mortality rates were higher among older patients than among younger patients. Age, increased plasma creatinine level, and total plasma exchange volume were independently associated with short-term mortality, whereas cardiac involvement was independently associated both with short- and mid-term mortalities.
Moreover, when compared with a control geriatric cohort of non-iTTP elders, iTTP 1-month survivors had a threefold higher risk of long-term mortality, independent of several survival risk factors. This shortened life expectancy in patients with a history of iTTP is consistent with a previous report from the Oklahoma group18 and could result from more prevalent long-term disorders including hypertension, depression, and cognitive impairment12,18 as well as iTTP-related sequelae, especially in older survivors. Nevertheless, the mechanisms underlying this excess of mortality in patients with a history of iTTP are still unclear but could be explained by a iTTP-induced decline of chronic conditions like chronic renal and cardiac failure or cognitive impairment. Data on functional status are lacking but all older patients enrolled in this study lived at home, which is an indirect marker of independence. Future works should especially address the possible deleterious synergistic effect of iTTP-related microthrombi combined with vascular wall remodeling events involved in chronic diseases such as diabetes and hypertension, as well as with senescent processes. iTTP and cardiovascular aging could therefore share common mechanisms of endothelial dysfunction including alteration of the nitric oxide pathway and inflammation.19-26 More generally, the occurrence of iTTP in a patient with a previously senescent endothelium could result in a more severe presentation with not only short-term but also more long-term consequences.
The management of iTTP in older patients needs to be adapted in light of the new available strategies in the field. Importantly, in the very near future, the anti–von Willebrand factor nanobody caplacizumab should become part of the standard treatment of iTTP on the basis of a recent positive randomized controlled trial.7 However, given the increased bleeding risk in patients receiving caplacizumab, there is an urgent need to assess more accurately the benefit-risk and the side effects associated with the use of caplacizumab in older patients as they receive more antiplatelet agents and/or anticoagulants. Moreover, caplacizumab could decrease the organ impairment at the acute phase,27 which, as older patients are less prone to recover from an acute injury, could also have long-term consequences in older iTTP survivors. Additionally, as preemptive rituximab strategy is becoming increasingly popular to prevent relapses, there is a need to assess the risk of repeated infusions of rituximab among those older patients who could suffer from an increased risk of infectious complications.28 Apart from the evaluation of such new treatment strategies in older patients, a comprehensive geriatric assessment including cognitive, functional, and nutritional statuses could describe the prognosis of iTTP in older patients more precisely.
A potential limitation of our study is that in our national registry, only certain iTTP cases with a documented severe ADAMTS-13 deficiency were reported. We may assume that frail people, like those living in nursing homes or long-term care facilities, are less diagnosed. Besides, data were not available for 310 patients, which could have introduced a bias if these patients were systematically different from those included. Nevertheless, data about the initial characteristics were available for 174 of them and comparisons between younger and older iTTP patients drew the same conclusions when these patients were included, which reinforces these comparisons. Moreover, although cardiac involvement was negatively associated with survival, we could not associate cardiac troponin levels with prognosis.5 However, this unexpected finding could result from a 30% rate of missing data for cardiac troponin in this study with a long period of inclusion. Our study included patients with an initial episode as well as relapses; it could therefore be argued that initial episodes and relapses should be considered separately. Although other works reported a trend toward less severe presentation in terms of symptoms, laboratory data, and the number of plasma exchanges required in their relapse episodes compared with their initial diagnosis, this did not translate into differences in clinical outcomes.29 On the basis of these statements, we and others consider that both in clinical practice and research, patients’ initial and relapse episodes should be viewed as comparable events in terms of the urgency of starting plasma exchange, as well as for enrollment in clinical trials.
Older patients with iTTP have a frequent atypical neurological presentation, which may delay the diagnosis. Practitioners should be aware of this in order to shorten the time to treatment, which could improve the prognosis in older iTTP patients. Promising new agents deserve evaluation in this specific population of patients characterized by substantially increased mortality.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Publication-related data will be shared on email request to the corresponding author.
The online version of this article contains a data supplement.
Acknowledgments
Patients were recruited with the help of the members of the Reference Center for Thrombotic Microangiopathies (CNR-MAT; listed in “Appendix”). The authors thank S. Thouzeau, S. Capdenat, S. Savigny (Laboratoire d’Hématologie, Hôpital Lariboisière, Assistance Publique–Hôpitaux de Paris [AP-HP], Paris, France), and S. Malot (CNR-MAT, Hôpital Saint-Antoine, AP-HP, Paris, France) for technical assistance.
This work was partly supported by a grant from the French Ministry of Health (Projet Hospitalier de Recherche Clinique, P120118, AOM12259). This work was also supported by the National Plan for Rare Diseases of the French Ministry of Health (Direction Générale de l’Offre de Soin [DGOS]). The Fondation pour la Recherche Médicale funded the preparation and initiation of the study. The Three-City Study was also supported by the Caisse Nationale Maladie des Travailleurs Salariés, Direction Générale de la Santé, Mutuelle Générale de l’Éducation Nationale (MGEN), Institut de la Longévité, Conseils Régionaux d’Aquitaine et Bourgogne, Fondation de France, Ministry of Research–INSERM Programme “Cohortes et collections de données biologiques,” Agence Nationale de la Recherche (ANR) PNRA 2006 and LongVie 2007, the “Fondation Plan Alzheimer” (FCS 2009-2012), and the Caisse Nationale de Solidarité pour l’Autonomie (CNSA).
The Three-City Study was conducted under a partnership agreement between INSERM, University Bordeaux 2 Victor Segalen, and Sanofi-Aventis.
Authorship
Contribution: R.P., C.R.-B., and P.C. designed the study, interpreted the results, and wrote the manuscript; S. Gourlain and K.P. performed the statistical analysis of the comparison with the Three-City Study population; M.J. performed the statistical analysis of the French registry for TMAs; Y.B., L.G., E.A., P. Poullin, F.P., E.M., C.P., M.H., S.S., A.W., A.S., S. Girault, Y.D., V.C., J.-F.A., C.M., P. Perez, J.-M.H., T.K., A.L., A.C.-R., C.D., D.C., A.V., and P.C. enrolled patients and collected clinical and laboratory information; and all of the authors critically reviewed and substantially improved the manuscript.
Conflict-of-interest disclosure: P.C. is member of the clinical advisory boards for Alexion; Ablynx, now part of Sanofi; Shire; and Octapharma. Y.D. and C.P. have participated in advisory boards for Ablynx, now part of Sanofi. The remaining authors declare no competing financial interests.
A complete list of the members of the Reference Center for Thrombotic Microangiopathies appears in “Appendix.”
Correspondence: Paul Coppo, Service d’Hématologie, AP-HP.6, 75571 Paris, France; e-mail: paul.coppo@aphp.fr.
Appendix
The members of the Reference Center for Thrombotic Microangiopathies (CNR-MAT) are: Augusto Jean-François (Centre Hospitalier [CH] Universitaire [CHU] Larrey, Angers, France); Azoulay Elie (Hôpital Saint-Louis, Paris, France); Barbay Virginie (CHU Charles Nicolle, Rouen, France); Benhamou Ygal (CHU Charles Nicolle, Rouen, France); Bordessoule Dominique (Hôpital Dupuytren, Limoges, France); Charasse Christophe (CH de Saint-Brieuc, Saint-Brieuc, France); Charvet-Rumpler Anne (CHU de Dijon, Dijon, France); Chauveau Dominique (CHU Rangueil, Toulouse, France); Choukroun Gabriel (Hôpital Sud, Amiens, France); Coindre Jean-Philippe (CH Le Mans, Le Mans, France); Coppo Paul (Hôpital Saint-Antoine, Paris, France); Corre Elise (Hôpital Saint-Antoine, Paris, France); Delmas Yahsou (CHU de Bordeaux, Bordeaux, France); Deschenes Georges (Hôpital Robert Debré, Paris, France); Devidas Alain (Hôpital Sud-Francilien, Corbeil-Essonnes, France); Dossier Antoine (Hôpital Bichat, Paris, France); Fain Olivier (Hôpital Saint-Antoine, Paris, France); Fakhouri Fadi (CHU Hôtel-Dieu, Nantes, France); Frémeaux-Bacchi Véronique (Hôpital Européen Georges Pompidou, Paris, France); Galicier Lionel (Hôpital Saint-Louis, Paris, France); Grangé Steven (CHU Charles Nicolle, Rouen, France); Guidet Bertrand (Hôpital Saint-Antoine, Paris, France); Halimi Jean-Michel (Hôpital Bretonneau, Tours, France); Hamidou Mohamed (Hôtel-Dieu, Nantes, France); Herbrecht Raoul (Hôpital de Hautepierre, Strasbourg, France); Hié Miguel (Groupe Hospitalier Pitié-Salpétrière, Paris, France); Jacobs Frédéric (Hôpital Antoine Béclère, Clamart, France); Joly Bérangère (Hôpital Lariboisière, Paris, France); Kanouni Tarik (CHU de Montpellier, Montpellier, France); Kaplanski Gilles (Hôpital la Conception, Marseille, France); Lautrette Alexandre (Hôpital Gabriel Montpied, Clermont-Ferrand, France); Le Guern Véronique (Hôpital Cochin, Paris, France); Loirat Chantal (Hôpital Robert Debré, Paris, France); Moulin Bruno (Hôpital Civil, Strasbourg, France); Mousson Christiane (CHU de Dijon, Dijon, France); Ojeda Uribe Mario (Hôpital Emile Muller, Mulhouse, France); Ouchenir Abdelkader (Hôpital Louis Pasteur, Le Coudray, France); Parquet Nathalie (Hôpital Cochin, Paris, France); Peltier Julie (Hôpital Tenon, Paris, France); Pène Frédéric (Hôpital Cochin, Paris, France); Perez Pierre (CHU de Nancy, Nancy, France); Poullin Pascale (Hôpital la Conception, Marseille, France); Pouteil-Noble Claire (CHU Lyon-Sud, Lyon, France); Presne Claire (Hôpital Nord, Amiens, France); Provôt François (Hôpital Albert Calmette, Lille, France); Rondeau Eric (Hôpital Tenon, Paris, France); Saheb Samir (Hôpital la Pitié-Salpétrière, Paris, France); Schlemmer Benoît (Hôpital Saint-Louis, Paris, France); Seguin Amélie (CH de Vendée, Vendée, France); Servais Aude (CHU Necker-Enfants Malades, Paris, France); Stépanian Alain (Hôpital Lariboisière, Paris, France); Vernant Jean-Paul (Hôpital la Pitié-Salpétrière, Paris, France); Veyradier Agnès (Hôpital Lariboisière, Paris, France); Vigneau Cécile (Hôpital Pontchaillou, Rennes, France); Wynckel Alain (Hôpital Maison Blanche, Reims, France); and Zunic Patricia (Groupe Hospitalier Sud-Réunion, la Réunion, France).