Patients with sickle cell disease (SCD) are now routinely living into adulthood, but SCD has deleterious effects on multiple organ systems which can lead to increased complications from illness. SCD patients generally auto-splenectomize in childhood secondary to infarctions from their hemoglobinopathy, thus increasing their risk of infection with encapsulated organisms such as S. pneumoniae. Although there are data to demonstrate that vaccination has drastically decreased the incidence of invasive pneumococcal disease (i.e. bacteremia or meningitis) in children, the situation for adults is less clear. There are no data to guide the decision to use conjugated and/or polysaccharide pneumococcus vaccines in adults. In addition, there are few data available on the efficacy of pneumococcal vaccination on non-invasive disease such as pneumonia. Two landmark studies have demonstrated the efficacy of polysaccharide-based pneumococcal vaccines in the general adult population to be approximately 56%. However, there are data to suggest that immune responses in SCD patients may be impaired, and thus responses to vaccines may be suboptimal.
Current sickle cell guidelines for pneumococcal vaccination, which are based on expert opinion, recommend one dose of Prevnar 13 (conjugated vaccine) followed by one dose of Pneumovax 23 (polysaccharide vaccine) with a booster of Pneumovax 23 at age 65. However, some clinicians choose to vaccinate every 5 years due to fear of waning immunity. There is a lack of data on which to base guidelines, and there are also no data nor any guidelines to help decide if patients needs additional boosters of vaccine.
Besides the potential for suboptimal immune responses in sickle cell patients, the standard definition used to define a responder to pneumococcal vaccine may not translate to protection from disease in the real world. Most studies define a responder as having a protective titer to 50-70% of the serotypes tested. However, this definition has no consideration for the prevalence of serotypes causing disease in the community. Therefore it's possible to have a patient who responds to 50% of the serotypes in the assay and is considered immune, but if those serotypes are all uncommon, then the patient may still be at high risk for serious disease. Determining a better way to identify patients at risk for pneumococcal disease and optimizing vaccination strategies to prevent this disease would help to improve the lives of patients.
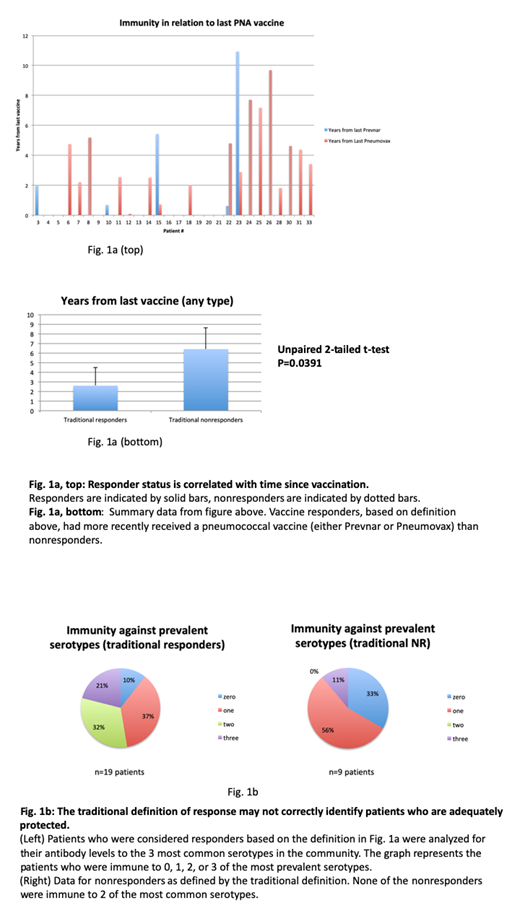
We performed a retrospective study to investigate immunity to pneumococcus in adult patients with SCD. We used the electronic medical record and collected data on patient demographics, sickle cell genotype, dates of previous pneumococcal vaccination (both conjugated and polysaccharide vaccines), quantitative antibody levels to individual pneumococcus serotypes, as well as information on comorbidities. In our sample of n=28 patients with SCD and available antibody data, 68% met a commonly accepted definition of immunity, which we defined by having an antibody concentration ≥ 1 mcg/mL for at least 50% of any of the serotypes tested. Immunity was inversely correlated with time from last pneumococcal vaccination, and it did not matter whether the most recent vaccine was the conjugated or polysaccharide product (Fig 1a). We then sought to analyze the data with consideration for the prevalence of various serotypes based on epidemiologic data published in The Lancet Infectious Diseases15,301-309 (2015). Interestingly, only 21% of patients who met the traditional definition of being a vaccine responder had protective titers to all 3 of the most prevalent serotypes tested, and 10% of patients who would traditionally be characterized as vaccine responders did not have sufficient antibody production to any of the 3 most prevalent serotypes tested in the assay (Fig. 1b, left). Of the 9 patients who were categorized as vaccine nonresponders based on the traditional definition, one subject was actually immune to all 3 of the most common serotypes in the community (Fig 1b, right), suggesting that he may actually be well-covered for pneumococcus in the real world. This study raises concern about the definition of immunity following vaccination, and highlights the challenge to identify which patients are at risk for disease. Future studies should examine how immunity wanes post vaccination and how the lack of immunity to prevalent serotypes might lead to clinical disease.
Lanzkron:Pfizer: Research Funding; Global Blood Therapeutics: Research Funding; Ironwood: Research Funding; HRSA: Research Funding; NIH: Research Funding; PCORI: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.