Background
Cancer is a known risk factor for venous thromboembolic (VTE) events. Thromboembolism occurs frequently during acute leukemia and the reported incidence of VTE in acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) are 5% and 6% respectively. However, majority of studies are conducted in Western population and data on VTE events in Asians with acute leukemia is scarce with only 1 published study.
Objectives
We aim to retrospectively evaluate the risk of thrombosis in Asian patients with acute leukemia and share our experience treating them.
Patients and Methods
This was a retrospective analysis on 257 adult patients who had presented to our centre from 1st January 2009 to 31st December 2017 with acute leukemia. There were 69 ALL, 9 acute promyelocytic leukemia (APL; M3 AML), 177 non-M3 AML and 2 acute biphenotypic leukemia (BAL). VTE events were identified to be those with clinical symptoms of VTE and had objective diagnostic imaging findings.
Results
Among the 257 patients, there were 65% Chinese (n=166), 26% Malays (n=67), 5% Indians (n=12), 4% others (Bengali, Emiratis, Eurasians and Filipinos). The overall incidence of VTE was 8% (n=21). The incidence of VTE was 16% in ALL (11 out of 69), 22% in APL (2 out of 9) and 5% in non-M3 AML (8 out of 177).
VTE was present at time diagnosis of leukemia in 0.7% of the patients (n=2). At 1 month from diagnosis of leukemia, the cumulative incidence (C.I) of thrombosis was 2.3% (n=6). At 6 months from diagnosis of leukemia, the C.I. of thrombosis was 5.8% (n=15).
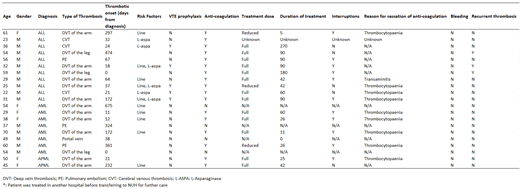
There were 48% line-related deep vein thrombosis (n=10), 19% non-line related deep vein thrombosis (n=4), 14% pulmonary embolism (n=3), 14% cerebral venous thrombosis (n=3) and 5% portal vein thrombosis (n=1). All 10 cases with line-related deep vein thrombosis had the line removed. All 3 cases of cerebral venous thrombosis occurred in patients with ALL on a L-Asparaginase containing regimen.
Seventeen out of 21 patients with VTE were treated with anti- coagulation. Four out of 21 patients did not receive any anti-coagulation due to thrombocytopenia. Of those who received anti-coagulation, 80% (n=14) received full dose anti- coagulation while 20% (n=3) received reduced dose anti- coagulation. In all 3 cases, the dose of anti- coagulation was reduced due to thrombocytopenia. Thirty-five percent received the full duration of anti- coagulation, 65% had anti-coagulation stopped earlier due to severe thrombocytopenia. The median duration of anti- coagulation received was 82 days.
The mortality rate due to VTE was 0.4% (n=1). This patient had massive pulmonary embolism with hemodynamic instability and demised within hours of diagnosis of pulmonary embolism. None of the patients had bleeding complications. Recurrent thrombosis occurred in 14% (n=3) of patients. All 3 patients had ALL and had completed the full duration of full dose anti- coagulation. None of the patients who did not receive anti-coagulation, received reduced dose anti-coagulation or had their anti-coagulation stopped earlier developed recurrent thrombosis.
Conclusion
The incidence of VTE in Asians with acute leukaemia is similar to that of the Western population. Main risk factors for thrombosis are that of line or chemotherapy related. The treatment of VTE remains challenging due to thrombocytopenia, with only 35% being able to complete the full course of treatment. However, despite so, there were no fatalities or recurrent thrombosis among those who were not started on therapy or did not have a full course of therapy. The role and duration of anti-coagulation needs to be explored in a prospective trial.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.