Background:
Patients with acute myeloid leukemia (AML) have dismal overall outcomes and survival is exceptionally poor in patients who experience relapse or are refractory (R/R) to frontline therapy. Since December 2018, combination therapy with hypomethylating agents (HMA) and venetoclax (HMA+Ven) has become standard frontline therapy for older patients or younger unfit patients. Moreover, it has been routinely utilized in patients experiencing relapsed or refractory AML yet response and outcome data is limited in patients with R/R disease. Thus, we investigated outcomes after HMA+Ven in patients with relapsed or refractory AML.
Methods:
We retrospectively annotated 72 patients who received treatment with HMA+Ven at Moffitt Cancer Center and Memorial Healthcare System between 2017 and 2019. Patients were divided into two subgroups: 1) initial remission therapy and 2) salvage therapy. Clinical and molecular data were abstracted in accordance with the Institutional Review Board approved protocol. Overall response rate (ORR) included patients achieving complete remission (CR), CR with incomplete count recovery (CRi), and morphologic leukemia free state (MLFS). Patients achieving CR, CRi, or MLFS were termed as responders (RES) and patients without CR, CRi, or MLFS were nonresponders (NRES). Fisher's Exact method was used to determine significance for categorical variables. Kaplan-Meier analysis was performed to determine median overall survival (mOS) and log-rank test was utilized to determine significance. All p-values are two-sided.
Results:
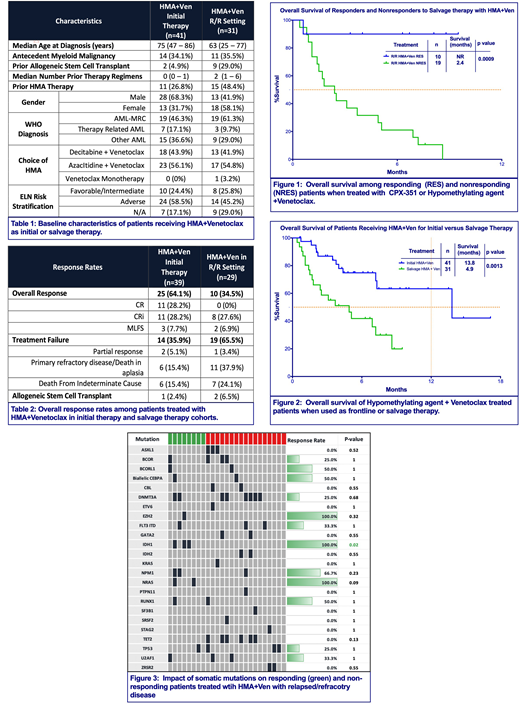
Out of 72 patients, 41 received HMA+Ven as initial therapy and 31 received it in the R/R setting. Baseline characteristics are outlined in Table 1. Median age was 63 years for patients with R/R AML with 58% female. In the R/R cohort, ORR was 34.5% with 0 (0%) patients achieving CR, 8 (27.6%) patients achieving CRi, and 2 (6.9%) achieving MLFS (Table 2). When compared to patients receiving HMA+Ven as initial therapy, ORR was significantly lower in the R/R cohort (64.1% vs. 34.5%, p=0.03). Among 31 patients in the R/R cohort, 6.5% (n=2) proceeded to allogeneic stem cell transplant (allo-SCT) after achieving CRi. European LeukemiaNet (ELN) risk stratification was known in 22 patients in the R/R cohort and ORR were similar in patients in the favorable/intermediate risk group (n=8) compared to adverse risk group (n=14) (37.5% vs. 28.6%, p=1.0). When compared to HMA+Ven used as initial therapy, ORR among the R/R cohort were not different among adverse risk groups (58.3% vs. 28.6%, p=0.10); however, ORR were significantly lower among patients with favorable/intermediate risk (100% vs. 37.5%, p=0.009).
At a median follow-up of 7.6 months (mo), mOS was 4.9mo in the R/R cohort with mOS among RES superior to NRES (not reached vs. 2.4mo, p=0.0009) (Figure 1). Moreover, mOS was inferior in R/R patients compared to initial therapy (4.9mo vs. 13.8mo, p=0.0013) (Figure 2). A total of 15 (48.4%) patients had HMA exposure prior to receiving HMA+Ven without apparent impact on mOS (3.7mo (prior HMA) vs. 4.9mo (no prior HMA), p=0.97).
The median duration of CR/CRi was 5.2mo and the median time to CR/CRi was 2.4mo. Based on ELN risk groups, mOS was not statistically different among patients with favorable/intermediate risk disease compared to adverse risk disease (8.6mo (fav/int) vs. 2.8mo (adverse), p=0.07).
Responses were also analyzed based upon somatic mutations (Figure 2). In patients with isocitrate dehydrogenase 1 and 2 mutations (IDH1/IDH2) compared to patients without IDH1/2, ORR were 60% vs. 25%, respectively (p=0.28) with no significant difference in mOS (7.2mo (IDHmut) vs. 3.1mo (IDHwt), p=0.38). Comparing patients with TP53 mutation to those without TP53 mutations, no significant difference in ORR (25% vs. 33%, p=1.0) or mOS (4.4mo vs. 6.9mo, p=0.0.84) was noted.
Conclusion:
Although combination therapy with HMA+Ven has yielded impressive responses as frontline therapy, response rates with this combination in the salvage setting are less encouraging with the possible exception of those patients with IDH1/IDH2 mutations. Nevertheless, responders to salvage HMA+Ven had a significant survival benefit compared to nonresponders, suggesting that this combination is a reasonable salvage option in patients with relapsed or refractory AML.
Padron:Incyte: Research Funding. Kuykendall:Incyte: Honoraria, Speakers Bureau; Celgene: Honoraria; Janssen: Consultancy; Abbvie: Honoraria. List:Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding. Lancet:Agios, Biopath, Biosight, Boehringer Inglheim, Celator, Celgene, Janssen, Jazz Pharmaceuticals, Karyopharm, Novartis: Consultancy; Pfizer: Consultancy, Research Funding; Daiichi Sankyo: Consultancy, Other: fees for non-CME/CE services . Sallman:Celyad: Membership on an entity's Board of Directors or advisory committees. Komrokji:JAZZ: Speakers Bureau; JAZZ: Consultancy; Agios: Consultancy; DSI: Consultancy; pfizer: Consultancy; celgene: Consultancy; Novartis: Speakers Bureau; Incyte: Consultancy. Sweet:Abbvie: Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Agios: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees; Celgene: Speakers Bureau; Jazz: Speakers Bureau; Incyte: Research Funding; Pfizer: Consultancy; Stemline: Consultancy. Talati:Jazz Pharmaceuticals: Honoraria, Speakers Bureau; Daiichi-Sankyo: Honoraria; Astellas: Honoraria, Speakers Bureau; Pfizer: Honoraria; Celgene: Honoraria; Agios: Honoraria.
Venetoclax is approved in combination with hypomethylating agents (azacitidine or decitabine) or low dose cytarabine for treatment of newly diagnosed AML in adults aged 75 years or older, or those who have comorbidities that preclude the use of induction chemotherapy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract