Introduction:
Patients (pts) with acute myeloid leukemia (AML) who are refractory to intensive frontline treatment have a dismal outcome. In case of ineligibility for allogeneic stem cell transplantation (HSCT), the median survival of chemo-refractory AML is about 2 months and less than 5% of these pts are alive after 1-year (retrospective analysis from the AMLSG database). To date, there is no universally accepted standard approach for the treatment of chemo-refractory AML in older pts. Several retrospective studies have assessed the role of hypomethylating agents in this patient group, but complete remission (CR) rates were disappointingly low (≤10%) when compared to first line treatment. The presented study represents a novel approach focusing on hematopoietic tissue reprogramming (i.e. anakoinosis) (ClinicalTrials.gov Identifier: NCT02942758).
Methods:
The initial dose-finding phase I of the study evaluated the combination of azacitidine (AZA) 75 mg/d s.c. for 7 days, repeated every 28-days, pioglitazone 45 mg/d p.o. continuously from day 1 and all-trans retinoic acid (ATRA). A modified 3+3 design has been used to establish the maximum-tolerated dose of ATRA. Patients have been enrolled at an ATRA dose of 45 mg/m²/d from day 1 to day 28 and 15 mg/m²/d continuously thereafter if no dose limiting toxicity (DLT) occurred until start of next cycle on day 29. The safety DLTs were defined as toxicities attributable to ATRA, expected or unexpected, except if these are likely associated with another cause.
Eligible patients had confirmed diagnosis of AML refractory to induction therapy and were not eligible for further intensive induction therapy or were not immediate candidates for allogeneic HSCT. The severity of adverse events was graded using the Common Terminology Criteria for Adverse Events (CTCAE) V. 4.03. The response to treatment was evaluated using standard criteria defined by the expert panel on behalf of the European LeukemiaNet and international working group (IWG) response.
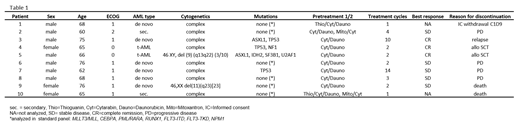
Results:
Ten pts were enrolled in the safety-run-in phase I (one pt withdrew informed consent on day 9 of cycle 1). Among all treated pts, the median age was 67 years (range, 62-76 years), and the majority of pts (70%) had an ECOG PS of 1 (see table 1). Two pts had secondary AML; another two pts had therapy-related AML (t-AML). Eight pts had a complex karyotype. Concerning safety, hematological adverse events (AEs) were the most common toxicities observed. Because pts with baseline cytopenia were included (leukopenia n=8; 80%; thrombocytopenia n=9; 90%), occurrences of many hematological AEs began before study drug initiation and were attributed to underlying hematologic disease. Common 3°/4° AEs included neutropenia (50%), anemia (50%), thrombocytopenia (30%), and infections (40%). 50% of pts experienced a serious AE; one 5° AE (gastric hemorrhage) occurred. No DLTs were observed. Five pts discontinued the study, with progressive disease (PD) or relapse being the most common reason for discontinuation. Concerning efficacy, 3 pts (30%) achieved a CR and one pt a long-lasting stable disease (14 months). Morphologic review showed signs of differentiation of blasts in responding pts, which has already been shown in in-vitro analysis. In line with this observation, one pt demonstrated resolution of fungal pneumonia during the study.
Conclusions:
In summary, the low-intensity, biomodulatory regimen of low-dose AZA, pioglitazone, and ATRA demonstrated a tolerable safety profile and encouraging signals for efficacy in pts with AML refractory to standard induction chemotherapy warranting further investigation.
S.T. and A.R. contributed equally to this abstract as senior co-authors.
Paschka:Novartis: Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses, Speakers Bureau; Astellas: Membership on an entity's Board of Directors or advisory committees; Agios: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses, Speakers Bureau; Abbvie: Other: Travel expenses; Amgen: Other: Travel expenses; Otsuka: Membership on an entity's Board of Directors or advisory committees; BMS: Other: Travel expenses, Speakers Bureau; Astex: Membership on an entity's Board of Directors or advisory committees, Travel expenses; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Other: Travel expenses; Takeda: Other: Travel expenses; Sunesis: Membership on an entity's Board of Directors or advisory committees. Döhner:Celgene, Novartis, Sunesis: Honoraria, Research Funding; AROG, Bristol Myers Squibb, Pfizer: Research Funding; AbbVie, Agios, Amgen, Astellas, Astex, Celator, Janssen, Jazz, Seattle Genetics: Consultancy, Honoraria. Thomas:Celgene: Consultancy, Other: Travel support, Research Funding, Speakers Bureau; Gilead: Membership on an entity's Board of Directors or advisory committees, Other: Travel support; Medigene AG: Consultancy, Other: Travel support; Novartis: Membership on an entity's Board of Directors or advisory committees, Other: Travel support, Speakers Bureau; Pfizer: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Medac: Other: Travel support; Janssen: Other: Travel support.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract