BACKGROUND AND AIMS
Real-world data on usage of 1st, 2nd and 3rd generation TKIs in CML are limited. Furthermore, current information on cost of CML treatment from a European perspective is scarce. Thus, this study followed four objectives: First, to get an overview over incidence and prevalence data. Second, to assess TKIs used in 1st and 2nd-line treatment, frequency of TKI switches and differences in cardiovascular comorbidities in different TKI patient groups. Third, to find predictors for a change of TKI treatment. Finally, to assess the costs associated with CML from a payer's perspective and to stratify these to the different health-care sectors.
METHODS
This observational study was based on the InGef research database, an anonymized representative claims dataset containing 4 million persons insured through the German statutory health insurances. Patients with an ICD-10 code C92.1, C92.2, C92.7 or C92.9 and with at least one prescription of a TKI, combined with a reimbursement code for diagnostic testing were included. Analyses were divided in an incidence cohort (ICD-10 code in at least two quarters between Jan 01, 2013 and Dec 31, 2014 and no corresponding diagnosis in 2012) and a prevalence cohort (diagnoses were assessed in 2012 (index period)). Patients were followed-up for three years in the incidence and up to five years in the prevalence cohort. In the prevalence cohort, patients could be counted multiple times when TKI was switched within the study period. Predictors for a TKI change were assessed using a multivariate logit model with backwards selection in the prevalence cohort for each follow-up year. Age, gender, comorbidities and medication were used as predictors. Annual health-care costs from a payer's perspective were included in the database and assessed in the prevalence cohort and stratified in inpatient, outpatient, pharmaceutical and other costs.
RESULTS
151 patients were included in the incidence cohort. This resulted in an extrapolated incidence and prevalence of 1,434 incident and 12,720 prevalent patients in Germany. Median age was 66 years and 46% of patients were female. Data on 1st line therapy was available for 124 patients and distributed across imatinib (N=52), nilotinib (N=44), dasatinib (N=12), hydroxycarbamide (N=11) and ponatinib/bosutinib (N=5). 22% of patients (N=32) switched TKI therapy at least once. Thereof, every second patient (N=18) switched to a 3rd line therapy. 43% of patients who started therapy on imatinib changed their treatment, compared to 34% in nilotinib and 14% in dasatinib. Median time to TKI switch was between 142 days (from imatinib to nilotinib) and 480 days (from nilotinib to dasatinib).
In the prevalence cohort, 636 patients were included with a median age of 65, 42% of patients were female. 423 patients (66.5%) had claims on existing or newly emerged cardiovascular diseases. No significant differences between TKIs were found, with 63.9% of imatinib (N=212), 69.6% of nilotinib (N=151) and 63.3% of dasatinib treated patients (N=81) had claims for existing or newly developed cardiovascular diseases (p=0.32).
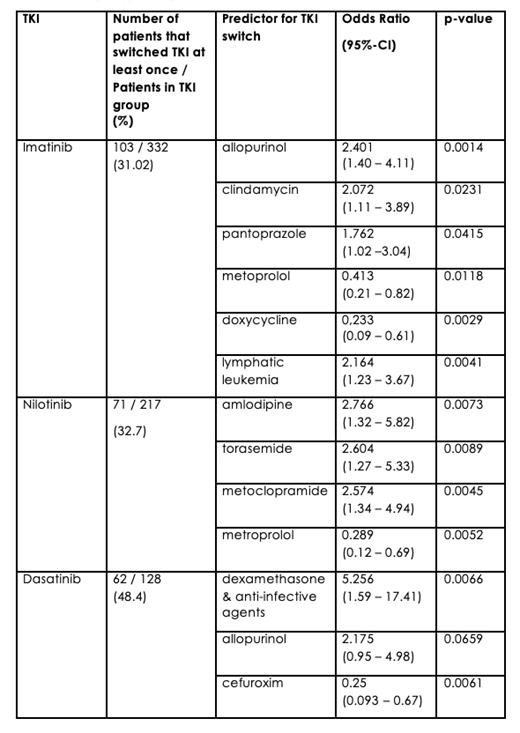
The most important predictors for therapy line change are displayed in table 1.
Mean annual costs for CML treatment were 58,230 €. Thereof, 56 % / 32,780 € were pharmaceutical (60-70% accounting on TKI), 28% / 16,383 € inpatient, 13% / 7,610 € outpatient costs. Median costs across different TKI therapies were 63,598 € for imatinib, 65,520 € for nilotinib and 88,342 € for dasatinib treated patients.
CONCLUSION
This study was the first German CML study based on a representative claims dataset. A difference in cardiovascular diseases across imatinib, nilotinib and dasatinib based on reported claims was not observed. Every fifth patient switched TKI therapy within the first three years after treatment initiation. Switches are more likely when signs of disease progression (e.g. comorbid ICD-10 code C91) or intolerability (e.g. prescription of anti-infective agents) are observable. To our knowledge, this is also the first study to report detailed cost data of CML in Germany. Costs between the TKIs differed only slightly with non-generic imatinib. With 12,720 prevalent CML patients, annual treatment costs amount to 740 million Euro in Germany.
Additional information: This study was supported by Incyte.
Saussele:Novartis: Honoraria, Research Funding; Pfizer: Honoraria; Incyte: Honoraria, Research Funding; BMS: Honoraria, Research Funding. Kaworski:Incyte: Employment. Vogelmann:Incyte: Consultancy, Honoraria. Schubert:Incyte: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.