Introduction:
Polycythemia vera (PV) is characterized by an increased red cell mass resulting in whole blood hyperviscosity, a strong predictor for thrombosis which remains a significant cause of morbidity and mortality1. Leukocytosis, thrombocytosis, and phlebotomy (PHL) rates are reported additive risk factors for thrombosis but their relative significance has been debated. PHL and cytoreductive therapy mitigates the risk of thrombotic complications. However, the relevance of these parameters remain insufficiently studied2,3.
Our primary objectives were to assess the significance of these risks and their associations with thrombosis. We also evaluated whether first-line interferon-α (rIFNα), hydroxyurea (HU), and phlebotomy-only (PHL-O) therapy is associated with reduced thrombotic risk.
Methods:
After IRB approval, 328 patients (pts) were evaluated after diagnosis according to PVSG criteria (1974-2007), published Weill Cornell criteria (2008-2016)4, or WHO 2016 criteria.
Demographics, clinical history, laboratory values, bone marrow findings, and genetic mutations were collected by querying our platform containing aggregated clinical data, the Observational Medical Outcomes Partnership Common Data Model5. Using intention-to-treat analysis, pts were assigned to a first-line therapy defined as continuous cytoreductive therapy for ≥1 consecutive year or PHL-O. Covariate differences between the first-line therapy groups at diagnosis were determined using χ2 tests for categorical variables. Overall survival (OS) was derived by the Kaplan-Meier estimator and comparisons of thrombosis risk were performed using a Cox proportional hazards model adjusted for clinically significant covariates such as age.
Results:
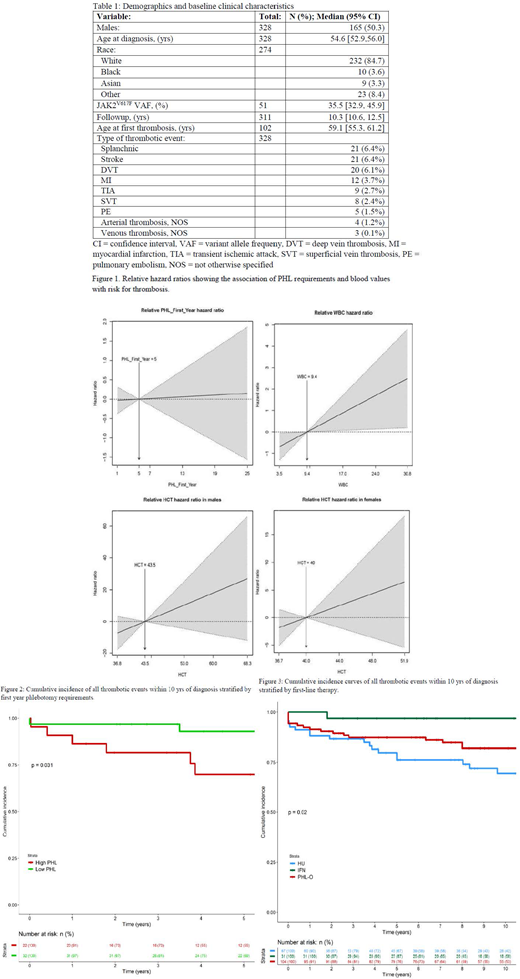
The characteristics of 165 men (50.3%) and 163 women (49.7%) with PV are shown in Table 1. Followup extended up to 45.0 years (yrs) with a median of 10.3 yrs. Median OS was 32.5 yrs. Splanchnic vein thrombosis, stroke, and deep vein thrombosis were the most common events. Median age at first event was 59.1 yrs.
Predisposing factors associated with thrombosis included uncontrolled HCT, increasing leukocytosis, and ≥5 PHL during the first year after diagnosis. Elevated HCT was the greatest contributor to thrombosis: males with HCT of 53.0% had thrombotic complications at 10 times the rate of those with HCT of 43.5% and females with HCT of 51.9% had a thrombosis at 6 times the rate of those with HCT 40.0% (Fig 1). Pts with leukocytosis (30.8x109/L) had a thrombosis at 2.5 times the rate of those with a white blood cell (WBC) value of 9.4x109/L. There was a weak association between platelet (PLT) count and thrombosis (data not shown).
The mean number of first-year PHL was 5.3±4.3; those pts requiring ≥5 had a thrombosis at 2 times the rate of those that required less (p=0.011). The difference in cumulative incidence of thrombotic events within 10 yrs was statistically significant for pts requiring ≥5 first-year PHL (p=0.031, Fig 2).
There was a significant difference in the cumulative incidence of thrombosis during the first 10 yrs of diagnosis dependent on first-line therapy (PHL-O: n=117, HU: n=84, rIFNα: n=40) (p=0.021, Fig 3). The apparent superiority of IFN over HU and PHL in this retrospective study is suggested by 10 year cumulative incidences of thrombotic events of 3.2, 18.0, and 30.6%, respectively.
Discussion:
There was a significant correlation between HCT, WBC count, and PHL requirements, but not PLT count, with thrombotic events. Elevated HCT was the most important risk factor. However, leukocytosis and first-year PHL rates also contribute as indicated by the higher hazard ratios. This suggests a need for cytoreductive therapy from disease onset. Our analysis shows that rIFNα reduces thrombotic risk when compared to HU and PHL.
Conclusion:
Multivariate analysis indicates that elevated HCT level is the most important parameter for correlation with thrombosis within the first 10 yrs of illness. However, WBC and PHL rates are also significant. Since thrombosis occurs from the time of diagnosis, our data suggest the need for cytoreductive intervention from onset. Analysis of the three most common first-year therapies shows that HU and PHL are inferior to rIFNα in reducing thrombotic risk.
Ritchie:Celgene: Other: Advisory board; Pfizer: Other: Advisory board, travel support; Celgene, Novartis: Other: travel support; Jazz Pharmaceuticals: Research Funding; Genentech: Other: Advisory board; agios: Other: Advisory board; Tolero: Other: Advisory board; AStella, Bristol-Myers Squibb, Novartis, NS Pharma, Pfizer: Research Funding; Ariad, Celgene, Incyte, Novartis: Speakers Bureau; Celgene, Incyte, Novartis, Pfizer: Consultancy. Silver:PharmEssentia: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.