Introduction: Defibrotide is approved for adult and pediatric patients with hepatic veno-occlusive disease/sinusoidal obstruction syndrome (VOD/SOS) with renal or pulmonary dysfunction after hematopoietic cell transplantation (HCT) in the United States and Canada and for patients aged >1 month with severe hepatic VOD/SOS post-HCT in the European Union. The recommended dose is 6.25 mg/kg every 6 hours given as a 2-hour intravenous (IV) infusion. Defibrotide has been shown in vitro to reduce endothelial cell (EC) activation and promote EC-mediated fibrinolysis. Post-HCT patients with VOD/SOS are often at a high risk for bleeding events. In a phase 3 study of patients with VOD/SOS post-HCT, rates of bleeding-related adverse events (AEs) with defibrotide were generally similar to matched historic controls (Richardson PG, et al. Blood. 2016;127[13]:1656-1665). To broaden our understanding of the risk of bleeding events associated with defibrotide treatment, this meta-analysis assessed the incidence and risk of bleeding-related AEs with defibrotide treatment in studies outside of the VOD/SOS and HCT setting, using published literature.
Methods: PubMed and Embase were searched from database inception through July 24, 2018 for studies using defibrotide (controlled trials with ≥1 arm assessing an intervention of interest, observational/retrospective studies, retrospective or post hoc analyses, and case series with ≥10 patients). Studies of patients with VOD/SOS or HCT, case reports with <10 patients, and reviews were excluded. Publications were evaluated for the presence of data on endpoints of interest, which included any bleeding-related event and overall safety or efficacy summaries; all studies with available data were included in the analysis. Overall bleeding rate was estimated for defibrotide and controls using the Freeman-Tukey double arcsine transformation and random-effects modeling (Stata Software). The risk ratio of bleeding was calculated using the Mantel-Haenszel method and random-effects modeling (RevMan 5.3 Software). Overall bleeding rate and risk ratio of bleeding were calculated from studies that used the IV defibrotide formulation; studies using oral or intramuscular formulations were excluded from these calculations.
Results: A total of 1,857 records were identified in the search; 124 studies reported on defibrotide and 19 contained data related to bleeding and were included in the analysis. Of the 19 included studies, 2 had >1,000 patients. An IV defibrotide formulation was used in 12 studies; the other 7 used intramuscular or oral delivery or more than one method of defibrotide administration. The most common indications were prevention of deep vein thrombosis (11 of 19) and treatment of thrombosis (3 of 19). Most studies (14 of 19) had 2 treatment arms; among these studies, heparin was the most common comparator (11 of 14). For the other 5 of 19 studies, 4 studies were single-arm and 1 study had 3 arms. The majority of studies (16 of 19) were conducted in adults; the other 3 studies did not specify patients' age. The most commonly administered defibrotide dose was 800 mg daily (14 of 19 studies). Bleeding rate and risk ratio of bleeding were calculated based upon data from the 12 studies that used IV defibrotide.
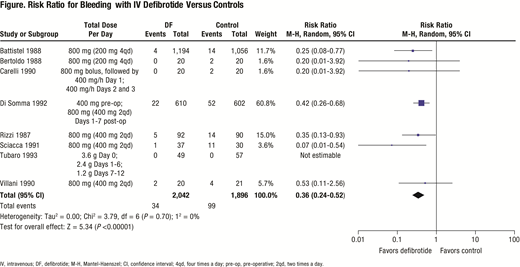
Rates of bleeding events reported in the 12 studies with IV defibrotide ranged from 0% to 10% in individual studies and the estimated overall bleeding rate was 1% (95% confidence interval [CI]: 0.00-0.03). In 10 studies with control treatments (9 calcium heparin, 1 urokinase), rates of bleeding events ranged from 1% to 37%, with 7 studies having rates ≥10%. Across the 10 control studies, the estimated overall bleeding rate for controls was 11% (95% CI: 0.05-0.20). Among the 8 studies with available data on IV defibrotide and controls (7 calcium heparin, 1 urokinase), the risk ratio for bleeding events with IV defibrotide versus controls was 0.36 (95% CI: 0.24-0.52; P <0.00001; Figure).
Conclusions: This meta-analysis of defibrotide use outside of the VOD/SOS setting suggests that the bleeding risk with defibrotide is low, and there is comparable risk of bleeding with defibrotide treatment versus controls such as heparin or urokinase. Important limitations of this analysis include variations in AE reporting across studies and the use of a defibrotide dose that is lower than the currently approved recommendation in the majority of studies.
Tappe:Jazz Pharmaceuticals: Employment, Equity Ownership. Aggarwal:Jazz Pharmaceuticals: Consultancy. Topaloglu:Jazz Pharmaceuticals: Consultancy. Iacobelli:Massimo Iacobelli: Consultancy.
The abstract describes a meta-analysis of defibrotide (indicated for VOD/SOS) in the non-VOD/SOS setting. As this analysis drew data from existing literature, no patients were administered defibrotide for off-label indications in the course of this analysis.
Author notes
Asterisk with author names denotes non-ASH members.