Background: Hospital readmission rates and acute care utilization among adults with sickle cell disease (SCD) are almost twice the rates of children. Adult patients may have complex medical and psychosocial needs that are not adequately addressed in fragmented healthcare systems. Few systems have implemented evidence-based, comprehensive care for SCD adults, shown to improve both medical and psychosocial outcomes in chronic diseases. Case management (CM) and community health workers (CHWs) are two evidence-based health management strategies that can help reduce health risks, reduce readmission rates, and improve patient-provider relationships.
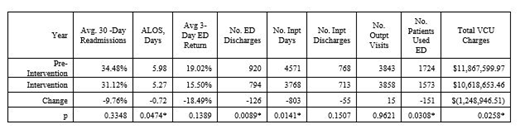
Methods: After years of attempting adult SCD CM with two MDs and one advanced practice provider (APP), Virginia Commonwealth University Medical Center (VCU) built upon a pilot study of CM and CHWs and implemented a multi-disciplinary Adult Sickle Cell Medical Home that assigned one of two CHWs for CM of the 50 highest SCD adult utilizers ranked by calendar year (CY) 2017 VCU charges, then by CY 2017 inpatient days. CHWs followed patients in and out of the hospital, and met with them at home. They were joined by a social worker who provided CM and behavioral therapy, an additional APP, and a project manager. This team met weekly. Medical Home leaders and quality improvement (QI) specialists enlisted other periodic caregivers to form QI teams with Medical Home workers focusing on behavioral health, ambulatory management, inpatient management, and emergency department (ED) management. A prior authorization specialist handled administrative access to opioids. Evaluation compared utilization during CY 2017 (pre-intervention) versus CY 2018 (intervention). For all patients we compared the average 30-day readmission rate, the average length of stay (ALOS), the average 3-Day ED return rate, the number of ED discharges, the numbers of inpatient days, inpatient discharges, and outpatient visits, the number of patients who used the ED, and total VCU charges. For the 50 highest utilizers, we compared the 30-day readmission rate, ALOS, total inpatient days and total VCU charges. VCU had no ambulatory SCD infusion unit, and the VCU ED did not have a special SCD rapid triage protocol. There was no control group. Analysis consisted of chi square and paired and unpaired t-tests.
Results: Among 567 SCD adults (Table), including 231 males and 336 females, ages 18 - 80, comparing pre-intervention to intervention, average utilization and VCU charges were either numerically or statistically significantly reduced, with the exception of outpatient visits, which remained flat. For the 50 highest utilizers, mean 30-day readmission rates were flat (45.98% vs 44.35%, p=0.7257), ALOS was significantly reduced (6.1 days vs 4.8 days, p<0.0001), inpatient days were reduced (206 days vs 106 days), and total charges were significantly reduced (25.43%, $5,297,323.73 vs $3,950,267.26, p=0.0037).
Conclusions: At VCU, a multi-disciplinary Adult Sickle Cell Medical Home that featured intensive CM and CHWs, but no infusion center or rapid ED triage, reduced annual utilization for adult SCD patients. CM program elements that were most effective should be studied in the future. A randomized controlled trial of CM and CHWs would strengthen evidence of their efficacy in improving utilization.
Smith:Novartis: Consultancy, Honoraria. Lipato:Novartis: Honoraria. Roberts:Truven Health Analytics: Consultancy; Community Health Network of Connecticut: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.