Background: Extra Corporeal Membrane Oxygenation (ECMO) is being used with increasing frequency in critically ill patients requiring cardiopulmonary life-support. The combined effects of critical illness, ECMO use, and systemic anticoagulation to prevent circuit thrombosis, induces a complex milieu of coagulation, fibrinolytic and platelet derangements. Both bleeding and clotting are expectedly the most frequent and dangerous complications of ECMO; in patients with active or high risk of major bleeding, the prospect of anticoagulation-free ECMO is attractive, although data is limited on the safety and efficacy of this practice. In order to better define the safety of anticoagulation-free ECMO, we performed the following systematic review.
Methods: We searched Ovid Medline for publications reporting use of ECMO without therapeutic-dose systemic anticoagulation of any kind for a minimum of 24 hours in adult patients, between the years 1977 to 2019. Studies using general venous thromboembolism prophylaxis were included. We included randomized control trials, cohort studies, case series, and case-control studies that contained sufficient patient-level data. Preclinical studies, meta-analyses, systematic reviews, narrative reviews, and reports involving patients under 18 years of age were excluded. Outcomes of interest collected included all bleeding and thrombotic events involving the patient or circuitry.
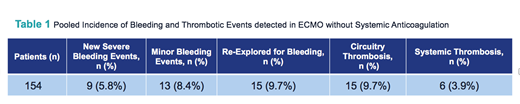
Results: 443 studies were identified through our search. After removal of duplicates, 441 records were screened. After exclusion, 23 full-text articles were assessed for eligibility. 2 of the full text articles were further excluded due to ambiguity regarding the time patients were off of anticoagulation. 21 studies were ultimately included in the systematic review. These included 8 case series and 13 individual case reports. All were single center studies. Data for a total of 154 patients among all 21 studies analyzed were reviewed. 96 adults were treated with veno-venous (vv) ECMO, and 58 were treated with veno-arterial (va) ECMO. Indications for ECMO included acute respiratory distress syndrome, diffuse alveolar hemorrhage, traumatic brain injury, intra-cranial hemorrhage, and lung transplant. Median total time on anticoagulant-free ECMO was 11.85 days among individual case reports, and 7.03 days for patients included in case series. Of the 154 patients, 9 (5.8%) had new, severe bleeding events, 13 (8.4%) experienced minor bleeding, and 15 (9.7%) were re-explored for bleeding. No new cases of intracranial hemorrhage were seen during ECMO without systemic anticoagulation. 15 patients (9.5%) developed circuitry thrombosis, and 6 (3.9%) developed systemic venous or arterial thrombosis. Full results are listed in Table 1.
Conclusions: Our systematic review found that anticoagulant-free ECMO was associated with relatively low rates of major bleeding, circuitry and patient thrombosis; the frequency of these events (5.8%, 9.5%, 3.9%, respectively) is similar, if not lower, than historically-reported rates in ECMO with anticoagulation (at least 16%, 10% and 18%, respectively). Of note, no new instances of intracranial hemorrhage were found, which is crucially important given the high associated mortality. Though based on a small number of patients, our review is valuable as it provides a new perspective on the prevailing theory that systemic anticoagulation is an absolutely necessary component of ECMO to prevent thrombosis. Evolving ECMO technology and improved overall care of critically-ill patients may be contributing to a less thrombotic blood microenvironment, which is typically attributed to inflammation, contact pathway and platelet activation. We acknowledge several limitations of our review, including the identification and inclusion of only non-randomized, retrospective studies, variable definitions and reporting of thrombotic and bleeding events, and likely non-negligible differences in ECMO technology, all of which precludes any definitive conclusions. Our findings are, however, hypothesis-generating; prospective, randomized trials would help better clarify the safety and efficacy of ECMO without anticoagulation, and address a unmet medical need by refining anticoagulation indications for critically ill patients on ECMO.
Shatzel:Aronora, Inc.: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.