Introduction: Blood transfusions are an important treatment modality for patients with either acute or chronic onset anemia such as trauma, sickle cell disease, and hematological malignancies. Transfusion poses a risk for alloimmunization, which may lead to potentially lethal transfusion reactions. A promising strategy to prevent alloimmunization is extensive matching on blood groups, yet this is a costly procedure and should be reserved for patients at highest risk for alloimmunization. Identification of genetic variants that increase the risk for alloimmunization might help to identify high-risk patients and could be used as a screening tool for patients receiving multiple transfusions.
Objectives: To summarize all available evidence on genetic risk factors for alloimmunization after blood transfusion.
Design: Systematic review with meta-analysis of observational studies. Studies were only included in the meta-analysis if polymorphisms were tested at least 3 times, and if ethnic background of the population and the control populations were comparable between studies.
Data sources: The online databases Embase, MEDLINE and the Cochrane Library were search for relevant articles with search terms: 1) transfusion, 2) alloimmunization 3) genetics. The search was last updated March 2018.
Eligibility criteria: 1) Primary study that assessed the association of genetic polymorphisms with transfusion related alloimmunization, 2) a human population, 3) studies with at least 50 patients, 4) full text availability.
Data extraction: Two reviewers independently screened articles for eligibility, extracted data using a standardized data extraction form. Extracted data included study setting, study population, participant demographics, baseline characteristics, study methodology, comparisons and outcome, and risk of bias.
Primary outcome measure: Alloimmunization after one or more blood transfusions.
Risk of bias assessment: The quality of the included studies was assessed by the Q-genie tool for genetic association studies.
Results: A total of 2045 cases and 24084 controls were derived from 18 genetic case-control studies that were included in this systematic review. Most commonly studied disease group was sickle cell disease (SCD) (8 studies). Three studies included patients with different diseases and seven studies did not report the underlying disease. Eleven studies identified the association of HLA polymorphisms with alloimmunization and 8 studies focused on non-HLA variants. Overall quality of the included studies was moderate (11 studies), 2 studies were of high quality, and 5 studies were ranked as poor.
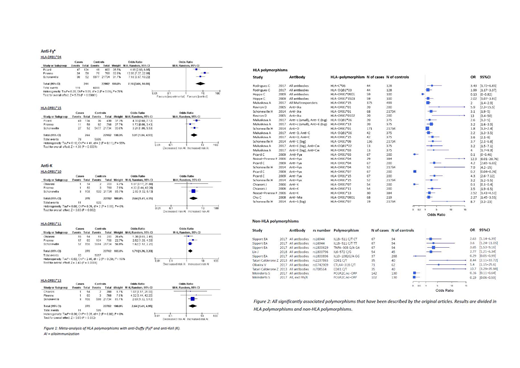
HLA-DRB1*04 (Odds Ratio 7.16, 95%CI 3.87-13.22, P<0.00001) and HLA-DRB1*15 (OR 3.01, 95%CI 1.84-5.53, P<0.0001) were by meta-analysis significantly associated with anti-Fy(a) formation, although there was considerable heterogeneity (I2=78% and 55% respectively). Moreover, HLA-DRB1*10 (OR 2.64, 95%CI 1.41-4.95, P=0.002), HLA*DRB1*11 (OR 2.11, 95%CI 1.34-3.32, P=0.001), and HLA-DRB1*13 (OR 1.71, 95%CI 1.26-2.33, P=0.0006) were overall associated with anti-Kell formation. Heterogeneity was less prominent with an I2 of 0%, 54% and 19% respectively (Figure 1). No other variants were eligible for meta-analysis.
Non-HLA variants were tested less extensively, as most variants were reported by only 1 study. Polymorphisms of genes in the immunomodulatory pathways were assessed most frequently. Of these variants, FC-gamma-receptor 2C.nc-ORF was associated with a decreased risk of alloimmunization in SCD (OR 0.26, 95%CI 0.11-0.64, p=0.003). All other associations that were described as significant by the original articles were summarized in Figure 2.
Discussion: There is limited evidence supporting the role of genetic risk factors for alloimmunization. The results of our meta-analysis suggest that several HLA polymorphisms potentially influence antigen presentation of the Duffy(a) and Kell antigen. Once confirmed by experimental studies, these polymorphisms could be used as a screening tool for the prevention of alloimmunization among frequently transfused patients.
Overall, the effect of genetic variants on alloimmunization has mostly been assessed by small studies, hampering reliable interpretation of the results. Future studies should include large and well-defined cohorts when performing genetic analysis on this complicated subject.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.