Introduction: Patients with diffuse large B cell lymphoma (DLBCL) arising from the testis have a relatively poor outcome. Age, stage and use of radiation and surgery are important prognostic factors in patients with primary testicular DLBCL. Additionally, the study by Gundrum et al suggested that laterality was also an important predictor of outcomes in patients with primary testicular DLBCL, with left side involvement being associated poorer prognosis. However, most patients included in the study by Gundrum et al were diagnosed in the pre-rituximab era, therefore, the role of laterality in the prognostification of patients with primary testicular DLBCL remains to be explored. In this study, the Surveillance, Epidemiology, and End Results (SEER) database was used to evaluate the prognostic roles of laterality in patients with primary testicular DLBCL.
Methods: Data from the SEER 18 Registries were used to conduct this study. Cases with newly-diagnosed testicular (International Classification of Diseases for Oncology, 3rd Edition [ICDO-3] codes 9823, sites: C62.0-C63.2) in the time period between 1973 and 2015 were included. Exclusion criteria included history of cancer, unknown laterality, unknown survival data and unknown cause of death. For each case we included age at the time of diagnosis, laterality (left, right, bilateral), SEER cause-specific death classification, survival months and vital status. Overall survival (OS) was defined as time from diagnosis to death or last follow-up and cancer-specific survival (CSS) was calculated as time from diagnosis to death from DLBCL or last follow-up. Survival curves were plotted by the Kaplan-Meier method and the log-rank test was used for comparison. P value was 2-sided and P<0.05 was considered to be statistically significant. All analyses were conducted using Graphpad Prism 6.
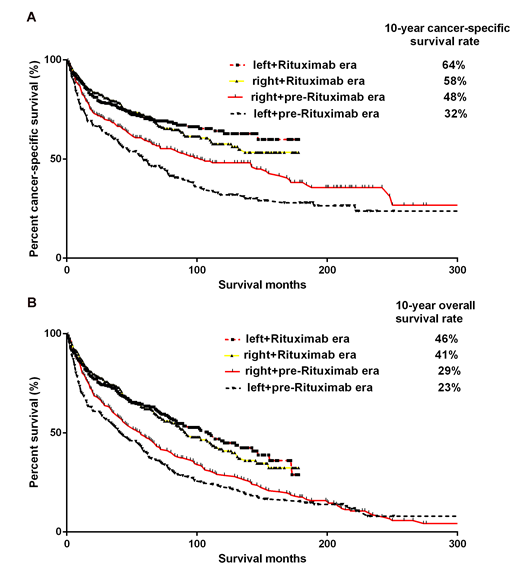
Results: A total of 1213 patients were included in this analysis. The median follow-up was 43 months (interquartile range[IQR]: 13-90 months). Of these patients, 372 patients were diagnosed from 1973-2000 (pre-rituximab era) and 841 patients were diagnosed from 2001-2015 (rituximab era). We found that patients with bilateral testis involvement had a significantly decreased CSS (median CSS: 53 vs. 142 months, P=0.0035) and OS (median OS: 32 vs. 77 months, P=0.0008) compared with those with unilateral involvement. Patients with left-side involvement had a similar CSS (median CSS: 136 vs. 153 months, P=0.2997) and OS (median OS: 76 vs. 80 months, P=0.7360) compared to those with right-side involvement. For patients with left-side involvement, patients diagnosed in the rituximab era had a significantly longer CSS(hazards ratio[HR]: 0.4140, 95% confidence interval[CI]: 0.3065 to 0.5593, P<0.0001) (Figure 1A)and OS (HR: 0.5522, 95% CI: 0.3926 to 0.6340, P<0.0001 ) (Figure 1B) than those diagnosed in the pre-rituximab era. For patients with right-side involvement, patients diagnosed in the rituximab era had a significantly longer CSS (HR: 0.7146, 95% CI: 0.5218 to 0.9029, P=0.0057) (Figure 1A)and OS (HR: 0.7116, 95% CI: 0.5407 to 0.8311, P=0.0011) (Figure 1B)than those diagnosed in the pre-rituximab era. The different HRs suggested patients with left-side primary testicular DLBCL benefited more from the introduction of rituximab. Additionally, the improvement in median OS from the pre-rituximab era to the rituximab era was 68 months for patients with left-side involvement but only 35 months for patients with right-side involvement.
Conclusion: our study demonstrated that laterality was not a prognostic factor for patients with primary testicular DLBCL. And the improvement in the prognosis from pre-rituximab era to rituximab era was more remarkable in primary testicular DLBCL patients with left-side involvement than those with right-side involvement. These data suggest primary testicular DLBCL from different sides had different responses to therapy and may have different biological characteristics.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.