Background:
Thrombolytic therapy is widely accepted for persistent hypotension or shock due to acute pulmonary embolism (PE), with randomized and observational studies demonstrating earlier hemodynamic improvement and possible mortality benefit. The extent to which thrombolytic therapy is used in urban versus non-urban settings is unclear.
Methods:
We conducted a retrospective cohort study of 92,706 (unweighted) and 180,189 (weighted) admissions with primary diagnosis of PE, for patient aged 18 years and above, that occurred in 2016, at all general acute-care hospitals within the 27 states included in the Nationwide Readmissions Database (NRD). Admissions for primary PE diagnosis and their respective severity levels (minor, moderate, major, extreme) were identified using the All Patient Refined Diagnosis Related Groups. We identified systemic and catheter-directed thrombolytic use using ICD-10-PCS codes. Hospital locations were classified as metropolitan (population ≥50K), micropolitan (10K-50K), and noncore (<10K). National estimates were calculated using post-stratification weights designed to compensate for any over- or under-represented hospital types in the NRD relative target universe of all hospitals in the U.S. PROC SURVEYFREQ and SURVEYLOGISTICS (SAS 9.4) were used to account for complex sampling design in variance calculations.
Results:
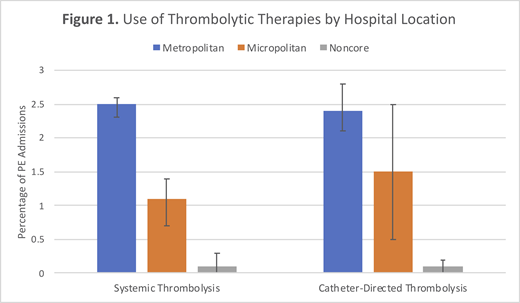
Of all primary PE admissions, 89.5% (95% CI, 88.7-90.2%) occurred at hospitals in metropolitan, 8.0% (95% CI, 7.3-8.7%) in micropolitan, and 2.6% (95% CI, 2.3-2.8%) in noncore areas. Rates of systemic thrombolytic use differed by location: 2.5% (95% CI, 2.3-2.6%) of admissions in metropolitan, 1.1% (95% CI, 0.7-1.4%) in micropolitan, and 0.1% (95% CI, 0-0.3%) in noncore areas (P<.001 for block test; Figure 1). Rates of catheter-directed thrombolytic use also differed: 2.4% (95% CI, 2.1-2.8%) of admissions in metropolitan, 1.5% (95% CI, 0.5-2.5%) in micropolitan, and 0.1% (95% CI, 0-0.2%) in noncore areas (P<.001 for block test). Differences persisted after adjusting for severity of illness for both approaches of thrombolysis (P<.001 in each block test of hospital location). Of patients with highest severity (major and extreme), systemic thrombolysis occurred in 4.0% (95% CI, 3.7-4.3%) of admissions in metropolitan, 1.9% (95% CI, 1.2-2.6%) in micropolitan, and 0.5% (95% CI, 0-1.1%) in noncore hospitals. In this same population, catheter-directed thrombolysis occurred in 2.4% (95% CI, 2.1-2.8%) of admissions in metropolitan, 1.5% (95% CI 0.5-2.5%) in micropolitan, and 0.1% (95% CI, 0-0.2%) in noncore hospitals.
Conclusion:
There was significant variation in use of systemic and catheter-directed thrombolysis for pulmonary embolism by hospital location. Thrombolytic therapy was rarely reported among noncore hospitals and occurred at a substantially lower rate at micropolitan than at metropolitan hospitals even when adjusted for illness severity.
Implications:
Efforts should be directed to understand drivers of urban-rural differences in use of thrombolytic therapies (e.g., knowledge, experience, support, resources) to identify potential levers to increase appropriate use of thrombolytic therapy particularly at hospitals in smaller, non-metropolitan communities.
Rosovsky:Janssen Pharmaceuticals: Consultancy, Research Funding; Bristol-Myers Squibb: Research Funding; Dova Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.