Introduction
In sickle cell disease (SCD), chronic anemia, hypoxia, and NO scavenging related to intravascular hemolysis contribute to diastolic dysfunction and pulmonary hypertension. Free hemoglobin and heme released during hemolysis cause oxidative stress and exacerbate vascular inflammation. Iron overload from frequent blood transfusions provokes reactive oxygen species and consequently cellular damage. We examined correlation of biomarkers reflecting major aspects of SCD patho-physiology (hemolysis, anemia, hypoxia, inflammation, and iron overload) with cardiopulmonary, renal, and liver dysfunction in an adult SCD cohort. The study provides observational evidence for etiologies of sickle cell organ damage by assessing the relative strength of outcome association for these biomarkers.
Methods
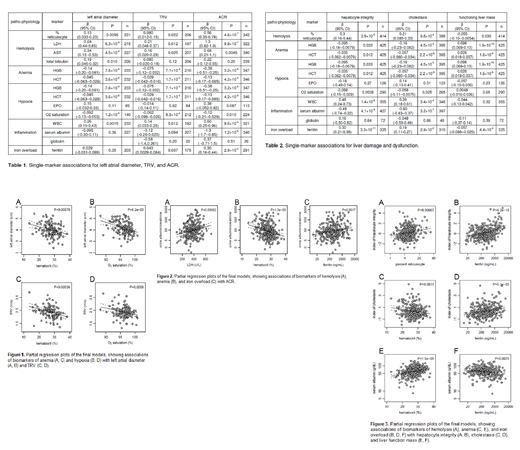
The study included 442 SCD patients with median age of 31 years, 77% with severe β hemoglobin mutation genotypes (HbSS, HbSβ0-thalassemia, HbSOarab) and 58% female. Biomarkers were identified for the SCD etiological conditions listed in Table 1. Primary cardiopulmonary outcomes were left heart enlargement (left atrial and ventricular diameter) and elevated systolic pulmonary artery pressure measured by tricuspid regurgitation peak velocity (TRV). The primary renal outcome was elevated urine albumin to creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2. Primary hepatic outcomes were hepatocyte integrity estimated as the first principal component (PC) of alanine transaminase (ALT) and aspartate aminotransferase (AST), cholestasis estimated as the first PC of alkaline phosphatase (ALP) and direct bilirubin, and functioning liver mass measured by serum albumin1. Clinical associations between biomarkers and primary outcomes first applied single marker regression with covariates of age, gender, and severity of β hemoglobin genotype. Significant biomarkers representative of the major SCD etiological conditions were then analyzed by multi-marker regression and model selection.
Results
Left atrial diameter showed significant associations with biomarkers of hemolysis (LDH, percent reticulocytes, AST, total bilirubin), anemia (HCT, HGB), hypoxia (HCT, HGB, O2 saturation), and inflammation (WBC) (Table 1). Left ventricular diameter had a profile of biomarker associations similar to left atrial diameter. TRV showed significant associations with biomarkers of hemolysis (LDH, percent reticulocytes, AST), anemia (HCT, HGB), hypoxia (HCT, HGB, O2 saturation), inflammation (WBC), and iron overload (ferritin) (Table 1). In multi-marker analysis, anemia and hypoxia (low HCT, low O2 saturation) associated with greater left atrial diameter and with high TRV (Figure 1).
Urine ACR significantly associated with biomarkers of hemolysis (LDH, AST, percent reticulocytes), anemia (HCT, HGB), hypoxia (HCT, HGB, O2 saturation), inflammation (WBC, serum albumin), and iron overload (ferritin) (Table 1). Impaired kidney function based on eGFR <60 mL/min/1.73m2 had a profile of biomarker associations similar to ACR. In multi-marker analysis, hemolysis (high LDH), anemia (low HCT), and iron overload (high ferritin) associated with increased ACR that indicates renal damage (Figure 2).
Hepatocyte integrity significantly associated with biomarkers of hemolysis (percent reticulocytes), anemia (HCT, HGB), hypoxia (HCT, HGB, O2 saturation), inflammation (WBC, serum albumin), and iron overload (ferritin) (Table 2). Cholestasis had a profile of biomarker associations similar to decreased hepatocyte integrity (Table 2). Functioning liver mass showed significant association with hemolysis (percent reticulocyte), anemia (HGB, HCT), and iron overload (ferritin) (Table 2). In multi-marker analysis, hemolysis (high percent reticulocyte) and iron overload (high ferritin) associated with decreased hepatocyte integrity (Figure 3A, 3B), whereas anemia (low HCT) and iron overload (high ferritin) associated with cholestasis (Figure 3C, 3D) and with low functioning liver mass (Figure 3E, 3F).
Conclusion
Our study indicated significant correlations of anemia and hypoxia with both left heart enlargement and elevated pulmonary arterial systolic pressure. Our study also underscores a significant impact of iron overload on renal and liver damages.
Acknowledgement
We thank CSL Behring Biotherapies for Life™ for their support of this study.
Saraf:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Pfizer: Research Funding. Gordeuk:Pfizer: Research Funding; Inctye: Research Funding; Imara: Research Funding; CSL Behring: Consultancy, Honoraria, Research Funding; Ironwood: Research Funding; Global Blood Therapeutics: Consultancy, Honoraria, Research Funding; Emmaus: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Modus Therapeutics: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.