Background: Salvage regimens for chemorefractory aggressive lymphoma achieve response rates of approximately 30%. Anti-CD19 CAR-T cells have demonstrated anti-lymphoma activity, but patients (pts) with rapidly progressive disease and urgent need for therapy have worse prognosis and many are not able to receive CAR-T cells in time. Decreasing the time from apheresis to infusion can make CAR-T cells available to pts with rapid progression of their disease. We present the results of a phase I clinical trial using on-site CAR-T manufacture for treatment of relapsed / refractory (r/r) B cell non Hodgkin lymphoma (NHL).
Methods: Adult pts with r/r CD19+ B cell lymphomas who failed ≥ 2 lines of therapy were enrolled. Autologous T cells were transduced with a lentiviral vector (Lentigen Technology, Inc, LTG1563) encoding an anti-CD19 binding motif, CD8 linker and tumor necrosis receptor superfamily 19 (TNFRS19) transmembrane region, and 4-lBB/CD3z intracellular signaling domains. GMP-compliant manufacture was done using CliniMACS Prodigy, in a 12-day culture. Dose escalation was conducted according to a 3+3 design. Lymphodepletion was done with cyclophosphamide (60mg/kg x 1) and fludarabine (25mg/m2/d x 3). Cytokine release syndrome (CRS) and CAR-T related encephalopathy syndrome (CRES) were graded using the Lee and CARTOX criteria, respectively.
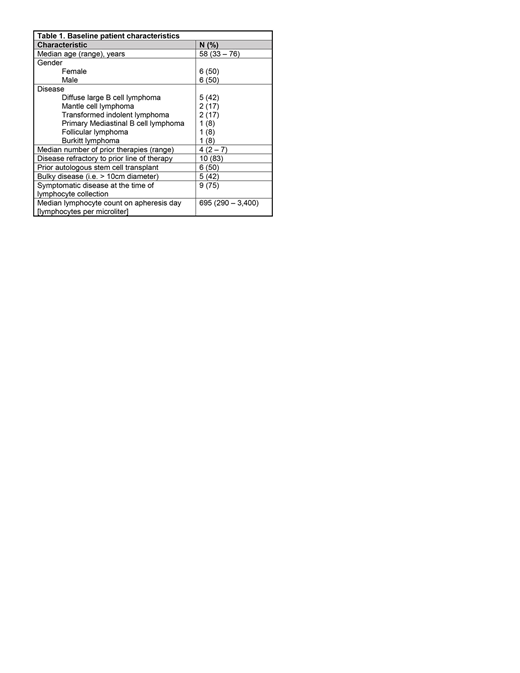
Results: As of July 30, 2019 , 12 pts were enrolled and treated. Baseline characteristics are listed in table 1. 10/12 pts were refractory to the prior line of therapy, 5 had bulky disease and 9 had symptomatic disease at the time of lymphocyte collection.
CAR-T cell product manufacture was successful in all pts. Median transduction rate was 48% [range 29-62] with and median culture expansion of 43-fold [range 30-79]. High dimensional flow cytometry showed the infused CD4 and CD8 CAR-T cells express a central memory and transition to memory - like profile, with enrichment for CD27 and high CCR7 expression. In addition, a subset of CD4 and CD8 CAR-T cells expressed effector transcription factors T-BET and GATA3 while CD4 CAR-T clusters express low levels of immune checkpoint blockers PD-1 and BTLA.
All enrolled pts received their infusion of anti-CD19 CAR-T cells. CAR-T cell doses were 0.5 x 106/kg (n = 4) and 1 x 106/kg (n = 8). Median apheresis to infusion time was 13 days [range 13-20], 10 products were infused fresh. CAR-T persistence, based on vector sequence, peaked in peripheral blood MNCs between days 14-21. All responding subjects have had CAR-T persistence on follow up PCR measurements (range 1 - 12 months). CAR-T cell dose did not have an impact in the time to peak in vivo CAR-T cell expansion or in the rate of CAR-T cell persistence.
Five pts experienced CRS. Grade 1 - 2 CRS was observed in 4 pts; whereas 1 pt died as a consequence of severe CRS in the context of bulky disease. Pharmacologic interventions for CRS included tocilizumab (n = 5), siltuximab (n = 2) and corticosteroids (n = 2). Two subjects presented grade 4 CRES with resolution after corticosteroids, no other grade ≥3 non-hematologic toxicity was observed. The most common all grade non - hematologic toxicity was fatigue, observed in 6 subjects. Hematologic toxicity was common, with grade ≥ 3 neutropenia observed in all subjects, with 4 subjects presenting grade 3 neutropenia without fever beyond day 30.
Among 11 pts evaluable for response, 8 pts have achieved complete response (CR) and one had partial response (PR). Two pts did not respond. For the intention to treat population (n=12), the CR rate was 67% and overall response rate (ORR) was 75%. Overall response rates were equal between both dose levels (75%), but CR rates were higher in pts treated with 1 x 106 CAR-T cells (75% vs. 50%).
Two pts have died, causes of death include progressive disease (n=1) and CRS (n=1). After a median follow up 3 months (range 1 - 12) all responding pts are alive; 1 subject relapsed 6 months after treatment with CD19+ disease and entered CR after anti-CD19 antibody drug immunoconjugate treatment.
Conclusions: In this phase 1 study, second generation anti-CD19 CAR-T cells with TNFRS19 transmembrane domain have potent clinical activity. The short manufacture times achieved by local CAR-T cell manufacture with the CliniMACS Prodigy enables treatment of a very high risk NHL population that would otherwise not be able to receive CAR-T products due to rapidly progressive disease.
Caimi:ADC Therapeutics: Research Funding; Celgene: Speakers Bureau; Genentech: Research Funding. Schneider:Lentigen Technology, A Miltenyi Biotec Company: Employment. Bakalarz:Genentech: Speakers Bureau. Kruger:Lentigen Technology Inc., A Miltenyi Biotec Company: Employment. Worden:Lentigen Technology, A Miltenyi Biotec Company: Employment. Kadan:Lentigen Technology Inc., A Miltenyi Biotec Company: Employment. Malek:Adaptive: Consultancy; Janssen: Speakers Bureau; Amgen: Speakers Bureau; Celgene: Consultancy; Takeda: Consultancy; Sanofi: Consultancy; Medpacto: Research Funding. Metheny:Takeda: Speakers Bureau; Incyte: Speakers Bureau. Dropulic:Lentigen Technology, A Miltenyi Biotec Company: Employment.
Clinical Trial of on - site manufactured CAR-T cells. This manufacturing process is under research.
Author notes
Asterisk with author names denotes non-ASH members.