Introduction:
Although opioids are the recommended treatment for acute pain management in sickle cell disease (SCD) patients, the opioid epidemic may have negatively affected the care of these patients in the emergency care settings. Literature suggested that ED physicians routinely overestimate opioid misuse in patients with SCD. Pennsylvania mandated Prescription drug monitoring programs (PDMP) in August 2016 which may affect ED opioid prescription among SCD patients. We evaluated the impact of that PDMP on opioid prescription in the management of acute pain for patients with SCD.
Method:
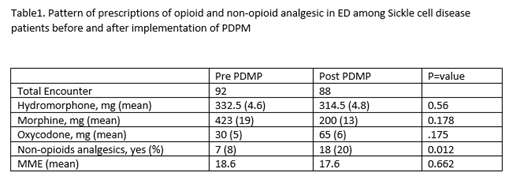
The data collection took place in the two community hospitals (Mercy Fitzgerald and Mercy Philadelphia Hospital) in Philadelphia. Participants were adults (aged ≥18 years) diagnosed with SCD who triaged for pain in the ED was included in the study. We grouped the encounter by year of PDMP implementation: prior to September 2016 (January 2016-August 2016), and after September 2016 (January 2017-August 2017) to collect patient records of a 6-month period and analyzed the data on number of visits, treatment types, opioid dispensing and total morphine milligram equivalents (MMEs) drug prescriptions during the ED visit. Paired t-test and chi square test were used to compare pre- and post-intervention results. Repeat encounters within 7 days period were excluded in the study.
Result:
The study included 180 qualifying ED visits (92 pre-intervention; 88 post-intervention). PDMP intervention was not significantly associated with reductions in the with opioid prescribing or the amount of prescribed MMEs. The mean age is 32.7 and 58% were male; and all were of African American race/ethnicity. However, prescriptions for non-opioid analgesics increased significantly during the same periods (p<0.012).
Conclusion:
During January 2017-August 2017, PDMP implementation was not associated with a change in opioid prescription among SCD patients in our community teaching hospitals in Philadelphia. The use of the PDMP would be expected to increase narcotic use by correctly identifying SCD patients as not having opioid misuse. The failure to increase narcotics suggests that the use of PDMP data to adjust prescribing for SCD patients is not adequate. As PDMP is crucial for addressing the opioid crisis, clinicians should also use PDMP data for more tailored care in SCD patients. Integration of palliative care could be more pragmatic approach in balancing opioid abuse and access to opioids for pain management among SCD patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.