Background: Median age at diagnosis for MM is 69 years with approximately 33% of the newly diagnosed MM (NDMM) patients aged ≥80 years (elderly). Yet, outcomes data and clinical trial participation in elderly MM patients are limited due to frailty and frequent comorbidities. Moreover, elderly patients are not candidates for stem cell transplant (SCT) and age is an independent poor prognostic marker, leading to disparate outcomes. The present study evaluated trends in outcomes and predictors of survival among elderly NDMM patients in the United States (U.S.).
Methods: Using Surveillance Epidemiology and End Results (SEER) database, we extracted data on age, gender, geographical regions, year of diagnosis, and vital status for elderly patients (age ≥ 80 years) with MM from 1975 to 2016. Relative survival (RS) was estimated as the ratio of observed survival to the survival expected in the general population in the absence of malignancy. This adjusted for the competing causes of mortality prevalent in elderly patients. Mortality rates were age-adjusted. To estimate trends in mortality, we estimated annual percentage change (APC) and average annual percentage change (AAPC) by fitting the data in the join point regression model using the NCI's Join point Regression Program, Version 4.5.0.1. A multivariate analysis was conducted to analyze the predictors of overall and myeloma-specific mortality among elderly patients fitting into Cox proportion hazard regression model.
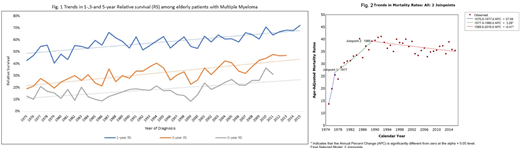
Results: A total of 17,265 elderly MM patients were eligible for the study. Majority were females (n=9,487, 55%), were non-Hispanic whites (NHW) (n=12,895, 74.7%) and were diagnosed in the Western region of the U.S. (n=8,541, 49.5%). The median age was 84 years (IQR 81-87). The median RS for the whole period (1975-2016) was 19.8 months with 1- and 5- year RS of 60.1% (95%CI: 58.8-61.3) and 20.9% (95%CI: 19.5-22.3) respectively. The median RS increased from 8.45 months in 1975 to 29.86 months in 2013. One and 5- year RS also increased from 42.7% (95%CI: 32.4-52.5) and 12.9% (95%CI: 5.8-22.7) in 1975 to a 1- and 5-year RS of 72.3% (95%CI: 65.4-78.1) and 31.1% (95%CI: 23.4-39.1) in 2013, respectively (Fig.1). However, the age standardized mortality rate for the whole period showed an increasing trend with an AAPC of 2.3 (0.5-4, P<0.001). On fitting joinpoint regression, 2 distinct joinpoints were identified, calendar years 1977 and 1989 (Fig 2). Most of the increase in mortality rate was noted in the period 1975-1989. Since 1989, the mortality rates have shown a decreasing trend which is marginal but statistically significant, with an APC of -0.41 (95%CI: -0.7- -0.1, p<0.001). On multivariate analysis, increasing age (p<0.001) and non-northeast location (p<0.01) were associated with higher overall and MM-specific mortality. Female gender was associated with lower overall mortality (p<0.001) but not myeloma-specific mortality. While "other" race/ethnicity (not NHW, non-Hispanic black; NHB or Hispanic) was associated with lower risk of overall and myeloma-specific mortality, NHB were associated with a lower MM-specific (p<0.001) but not overall mortality.
Conclusions: Our results suggest that although RS has improved significantly in the elderly patients, the mortality rates have not changed drastically over the years. Besides, factors like advancement in diagnosis and treatment which have improved RS, early diagnosis (leading to lead time bias) may also be contributing. Furthermore, there are several gender-specific, geographic and racial/ethnic disparities in outcomes of elderly MM patients, which need to be assessed prospectively. Although, a small decline in mortality rates in the more recent time is promising, further studies are warranted on interventions including aggressive supportive care directed at elderly patients with MM, so that MM survivorship can be improved. There should be strong consideration to increaseenrollment of the elderly in prospective clinical trials so that evidence-based guidelines can be developed.
Manochakian:Takeda: Membership on an entity's Board of Directors or advisory committees; Guardant Health: Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Membership on an entity's Board of Directors or advisory committees; Novocure: Membership on an entity's Board of Directors or advisory committees. Chanan-Khan:Merck: Research Funding; Ascentage: Research Funding; Millennium: Research Funding; Jansen: Research Funding; Mayo Clinic: Employment; Pharmacyclics: Research Funding; AbbVie: Research Funding; Xencor: Research Funding. Ailawadhi:Janssen: Consultancy, Research Funding; Takeda: Consultancy; Celgene: Consultancy; Amgen: Consultancy, Research Funding; Cellectar: Research Funding; Pharmacyclics: Research Funding. Off Label Use: Do not remove- this information is relevant to Abstract ID 125629: TAK-169 is a dimeric fusion protein of an anti-CD38 antibody single chain variable fragment fused to a modified Shiga-like toxin-A subunit..
Author notes
Asterisk with author names denotes non-ASH members.