Introduction: There is limited consensus on the optimal regime and benefit of fluid and oxygen therapy when treating vaso-occlusive episodes (VOEs) in children with sickle cell disease (SCD). The purpose of this study was to investigate the current prevalence of intravenous fluid and oxygen therapy when treating VOEs in children with SCD in a large tertiary hospital in London, UK and analyse the clinical outcome of these patients, in order to design a future study to determine optimum use of fluid and oxygen therapy in children presenting with VOE.
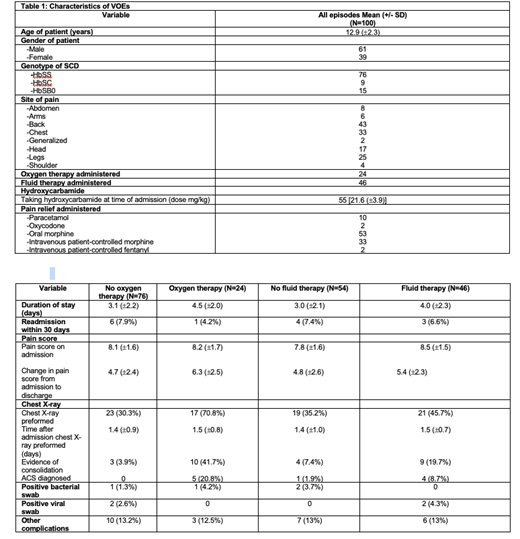
Methods: We studied a random selection of 100 vaso-occlusive events in paediatric sickle cell patients resulting in hospital admission between 2008-2019. All patients received assessment and initial treatment according to established hospital guidelines at the emergency department (ED) and were subsequently admitted to an inpatient ward. Baseline clinical and laboratory information, alongside data on the admission, duration, treatment and clinical outcome of each VOE were recorded. Data were compared between therapy and non-therapy groups.
Results: Out of 100 VOE events, 46 were given fluid therapy and 24 were given oxygen therapy. All cases of VOE on fluid therapy were treated with IV dextrose saline (0.5% dextrose and 0.45% NaCl), and the average rate of fluid given was 71.4 ml/kg/24hour (±20.7). No intravenous bolus of normal saline was administered. Fluid therapy was associated with a higher reduction in pain score points at discharge (5.4±2.3 vs 4.8±2.6). However, it was also associated with more chest x-rays (CXR) positive for consolidation (20% vs 7%) and more acute chest syndrome (ACS) diagnosis (9% vs 2%). The mean oxygen saturation in air of patients given oxygen therapy in ED was 96.6% (±4.8) and those that were not given oxygen therapy in ED was 98.2% (±1.6). Oxygen therapy was associated a higher reduction in pain score points at discharge (6.3±2.5 vs 4.7±2.4). However, in the oxygen therapy group, more CXRs were undertaken (71% vs 30%), more CXRs were positive for consolidation (42% vs 4%) and there was more (ACS) diagnoses (21% vs 0%).
Conclusion: These data reveal that about half of children presenting with VOEs received intravenous fluid therapy and about a quarter received oxygen therapy for the treatment of VOEs in this single-centre study. These therapies were associated with positive and negative impacts on clinical outcome. This highlights the need for randomised-controlled trials to evaluate the optimal regime for such therapies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.