Newborn sreening (NS) for sickle cell disease (SCD) is effective in reducing early mortality and morbidity through education, prevention of infections and strategies to prevent stroke in children at risk of cerebral vasculopathy. Universal NS was implemented in all Brussels maternity wards since 2000. All identified children with SCD benefited from comprehensive medical care in dedicated centers.
This retrospective study included all children with SCD diagnosed through NS and born between January 2000 and December 2005 (Group 1) and between January 2010 and December 2015 (Group 2) followed at Hôpital Universitaire des Enfants Reine Fabiola (Brussels, Belgium). Only patients whose parents consented to be recorded in the Belgian SCD database were eligible for this study. The aim of our study was to compare the outcome of 2 NS cohorts born at 10 years of interval.
Demographic data, baseline hematological values and clinical events, occurrence of cerebral vasculopathy and prescription of disease-modifying treatments during the first 5 years of life were compared between both groups. Data were collected until March 1, 2019.
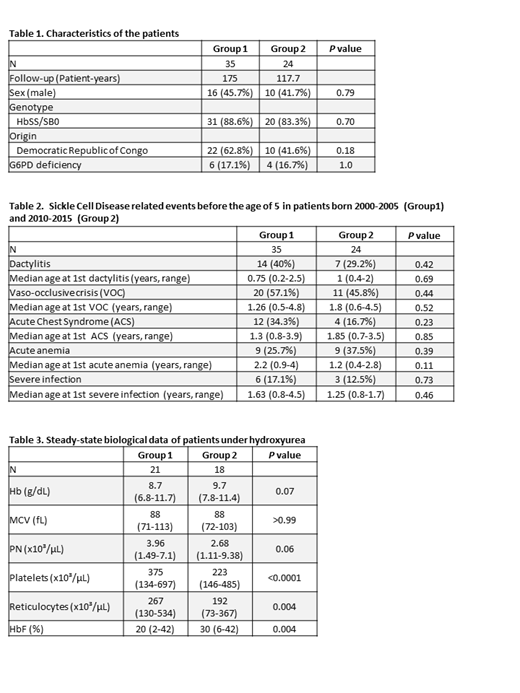
59 patients were identified for this study (35 in Group 1 and 24 in Group 2). Their characteristics are detailed in Table 1. Two patients in Group 2 did not completed the full 5-year evaluation period.
Among these 59 patients, 77.9% patients developed at least one SCD clinical event before the age of 5. The number of patients who developed a specific clinical event as well as their age at this first event was the same between the 2 groups (Table 2). The hospitalization number and hospitalization days were not statistically different in the 2 groups (5 vs 4 hospitalizations during 5 years and 19 vs 17 days of hospitalization between Groups 1 and 2 respectively). 3 patients presented an overt stroke (1 in Group 1 and 2 in Group 2) with a global incidence of 1.02 stroke per 100 patient-years. No death was reported in both groups.
The proportion of patients with abnormal transcranial doppler velocities decreased slightly in Group 2 (14.3% vs 8.3%, P=0.69) with more conditional velocities (5.7% vs 20.8%, P=0.10) but it was not statistically significant.
60% of patients in Group 1 were treated with hydroxyurea (HU) compared to 75% in Group 2 (P=0.27). HU was introduced at a median age of 2.5 (0.9-4.8) and 2.3 (0.8-4.8) in Groups 1 and 2 respectively (P=0.79). One patient from each group underwent an hematopoietic stem cell transplantation at 4.9 and 3.5 years.
Hematological values were not different in the 2 groups excepted for platelets count, which were significantly lower in Group 2 (421 x 10³/µl vs 331 x 10³/µl, P=0.03). Moreover in patients under HU, platelet and reticulocytes count were statistically lower and HbF higher in Group 2 compared to Group 1 (Table 3).
Nearly 80% of patients presented a clinical event before the age of 5. This is comparable to what is described in the literature. The Kaplan-Meier survival curves were not statistically different in both groups for the occurrence of a first dactylitis (P=0.52), a first vaso-occlusive crisis (P=0.22) and acute chest syndrome (P=0.37). No more difference was observed for acute anemia (P=0.43), severe infection (P=0.35) or patients under HU (P=0.40).
Even if the number of patients on hydroxyurea is not statistically higher in Group 2, a better exposure to hydroxyurea is attested by the significant changes in some biological parameters.
The limits of this study are the small size of our single center cohort and the exclusion of patients not recorded in the Belgian Registry because of lack of parental consent. This last point might create a bias by selecting patients whose parents are more prone to participate actively in the comprehensive care program.
This periodic evaluation is essential to ensure the quality of care of patients and to measure possible changes in the management.
Comprehensive care developed in our tertiary center had been already effective since 2000. Physicians not only tend to prescribe more hydroxyurea in young symptomatic patients, but also routinely adjust the dose to reach the maximal tolerated dose. Moreover adherence to treatment has been achieved through continuous education.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.