Drug-induced immune thrombocytopenia (DITP) is a rare and often overlooked cause for thrombocytopenia. It is a particularly difficult diagnosis given its rarity and because at least 100 different medication have been implicated. Cases of piperacillin-tazobactam-induced DITP have sparked growing interest given how common this antibiotic is used. Few studies, however, have defined the specific moiety causing the suspected DITP by serologic testing. When this has been done, only piperacillin has been implicated. Here, we describe the first case of DITP in which tazobactam was implicated by serologic studies.
Case
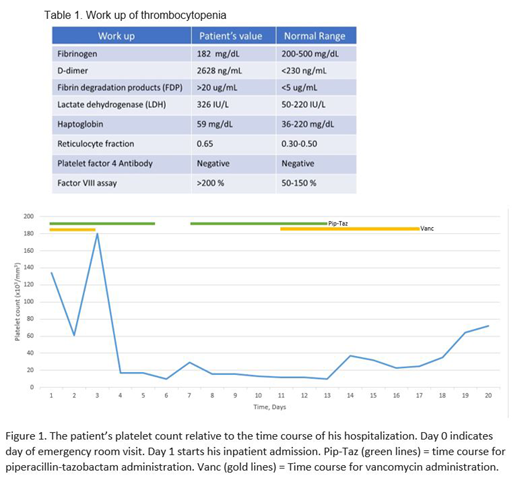
A 62 year-old-male with a past medical history of Crohn's disease, alcohol use disorder and chronic obstructive pulmonary disease (COPD) presented to the hospital with bilateral lower extremity pain and redness, and diffuse abdominal pain for 1 week. His home medications included pravastatin, meloxicam, pantoprazole and adalimumab. Physical exam, lab testing and imaging studies provided evidence for lower extremity cellulitis, multifocal pneumonia and possible colitis. In the Intensive care unit the patient was started on broad-spectrum antibiotics (vancomycin and piperacillin-tazobactam). He developed new onset thrombocytopenia to <20 K/UL (>50% drop within 72 hours) by hospital day 3, and vancomycin was discontinued.
A peripheral smear showed no evidence of schistocytes or platelet clumps. Subcutaneous heparin was discontinued and supportive care with vasopressors, antibiotics and RRT was continued. Patient's septic shock improved, and he was eventually weaned off the vasopressor support. However, his thrombocytopenia persisted which prompted further workup as shown in Table 2.
After initial workup remained unrevealing, piperacillin-tazobactam was discontinued and he was started on cefepime on hospital day 11. On day 12, his thrombocytopenia started to improve and showed an upward trend over next 48 hours. At this point antibiotic associated thrombocytopenia was highly suspected so antibiotic specific antibodies to piperacillin-tazobactam were requested. Platelet count on the day of discharge (hospital day 18) was 72 K/UL (Figure 1).
IgM antibodies that reacted with normal platelets only when tazobactam was present in the reaction mixture were identified in laboratory testing performed by the Platelet and Neutrophil Immunology Laboratory of Versiti-BloodCenter of Wisconsin.
Discussion
Serologic findings made in this very complex case indicate that severe thrombocytopenia was caused by an IgM antibody that recognized normal platelets only in the presence of tazobactam. Tazobactam is almost invariably given with piperacillin to inhibit bacteria-derived penicillinase and prolong the lifespan of piperacillin in vivo but, although numerous cases of piperacillin-induced thrombocytopenia have been described, this is the first report in which tazobactam has been documented as the trigger for immune thrombocytopenia. While tazobactam, like piperacillin, contains a beta-lactam structure, tazobactam-specific antibiotic testing may have implications on choosing future antibiotic therapies (particularly penicillins) for a patient. DITP occurring in the ICU can often be over-looked because patients tend to be critically ill and there may be many other reasons for a low platelet count. It is important to keep this diagnosis in mind whenever severe thrombocytopenia develops. Additionally, further work may seek to understand whether a patient's penicillin allergy may be specific to a moiety such as tazobactam, allowing continued use of other types penicillin-class drugs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.