Background: Management of surgical procedures in people with hemophilia (PwH) has always been a major concern. Insufficient hemostatic control might be an important cause of morbidity and mortality. However, the success of surgical procedures does not only depend on appropriate replacement of the missing factor. Pre- and post-operative interventions, laboratory monitoring, care and rehabilitation of the patient are important. Therefore, surgical procedures in hemophilia patients should be performed in full-fledged hospitals capable of providing a multidisciplinary approach as a "Comprehensive Hemophilia Treatment Center". The aim of our study is to evaluate the outcomes of major surgical procedures (MSPs) among PwH who were followed at Cerrahpasa Medical Faculty.
Methods: All MSPs performed on PwH between 2004 and 2017 were included. Baseline activated partial thromboplastin time (aPTT)and factor levels prior to MSP, inhibitor screening and (if any) the inhibitor titration results together with complete blood count, blood group and liver function tests were retrospectively obtained from patient files. The type of MSP, amount of factor concentrates given prior to, during and after the operation, the factor levels and aPTT results following factor replacement; complications developing during or after surgery, and information on the type of treatment modality prior to surgery (on demand vs. prophylaxis) were noted. The amount of factor concentrates administered to patients was determined in units per kilogram.
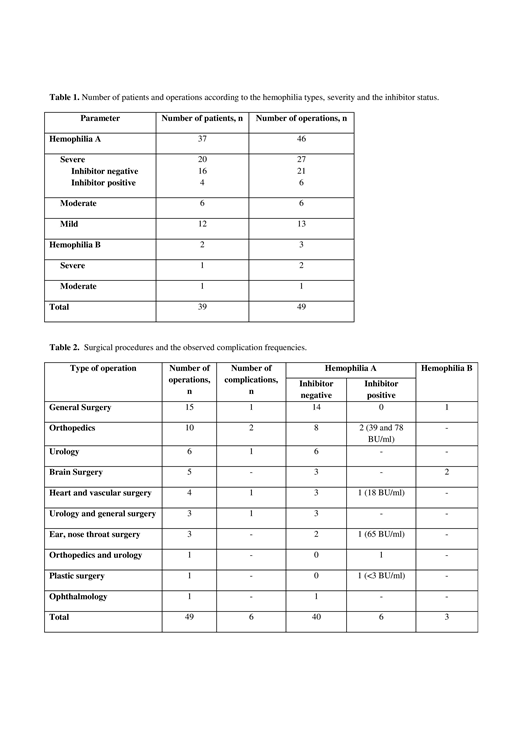
Results: Of the 39 patients included in the study (37 hemophilia A and two hemophilia B) 20 were severe, 7 were moderate and 12 were mild hemophilia (Table 1). The median age at the time of MSP was 37 (20-61) years. A total of 49 MSPs were performed, two patients had 3 surgeries, six patients had 2 surgeries, and 30 patients had one surgery. Fifteen surgical procedures were performed in two, one surgical procedure was performed in three, and 33 operation procedures were performed in one operation area. There were no significant differences in complication rates between hemophilia types (A vs. B), severities (severe vs. moderate vs. mild) and number of operated regions (1 vs. >1). In our study, general surgery (n=15) and orthopedic (n=10) operations were the most frequently performed MSPs (Table 2). There was no significant difference in complication rates among surgical branches. Complications were observed in a total of 6 (12%) MSPs, and one patient was deceased due to sepsis. Complication rates were 16% and 11% for MSPs done in PwH with and without inhibitors, respectively (p=non-significant). Factor consumption (U/kg) was highest in patients undergoing orthopedic surgery, followed by cardiovascular and neurosurgical operations. Factor utilization was significantly less for operations done in general surgery, urology and ear, nose and throat departments (p<0.001). There was a significant positive correlation between factor consumption and duration of hospitalization (r = 0,690; p <0.001). The data on the type of factor were available in 36 MSPs. Surgical procedures were carried out using plasma-derived and recombinant factor concentrates only in 26 and 5 patients, respectively. In the remaining 5, plasma-derived and recombinant factor concentrations were alternately applied. No statistically significant difference was noted with regard to the type of the factor used (plasma-derived, recombinant and plasma-derived/recombinant) and the duration of hospitalization or the complication rate. Number of days spent in the hospital were significantly higher in patients with complications than those without (16 vs. 9.5 days; p=0.003).
Conclusion: The results of our retrospective study, being consistent with the current literature, clearly demonstrates that, in experienced comprehensive care centers MSPs can effectively and successfully be performed in PwH, even in those with inhibitors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.