Introduction: Anemia is a common and unfortunate consequence of chemotherapy; patients receiving a variety of chemotherapy regimens often develop chemotherapy-induced anemia (CIA), which contributes to poor outcomes including increased mortality. Prompt and effective treatment of CIA is essential to prevent fewer chemotherapy dose delays and reductions. Optimal therapy of CIA is controversial and involves the solitary and combined use of intravenous iron, red blood cell (RBC) transfusions, and erythropoietin stimulating agents (ESAs). Despite the baseline coagulopathies present in patients with malignancy, administration of both RBC transfusions and ESAs is independently associated with venous thromboembolism (VTE). It remains unknown whether the risk of VTE in patients with CIA is greater among patients who receive RBC transfusions or ESAs.
Methods: A retrospective study analyzed 13,334 patients in the University of Pennsylvania Health System with malignancies of various type, stage, and histopathology who developed CIA between 1998-2017. Using multivariate Cox regression, we determined adjusted hazard ratios (and corresponding 95% confidence intervals) of VTE development after adjusting for RBC and ESA intervention (all during the 90 days following CIA diagnosis).
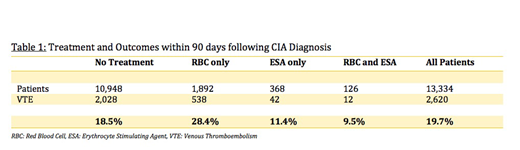
Results: (Table 1) Among the 13,334 patients with CIA, 10,948 patients did not receive any therapy during the 90-day period for their anemia (neither RBC nor ESA), 1,892 received RBC transfusion, 368 received ESA, and 126 patients received both. Among all patients, 2,620 (19.7%) developed a VTE within the 90-day period. VTE risk following RBC transfusion (HR=2.18, 95% CI 1.98-2.39, p<0.001) was approximately four-fold the VTE risk following ESA administration (HR=0.55, 95% CI 0.42-0.72, p<0.001).
Conclusion: While both RBC transfusion and ESA administration are associated with VTE, our data suggests a greater risk of VTE development with RBC transfusion as compared with ESA administration.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.