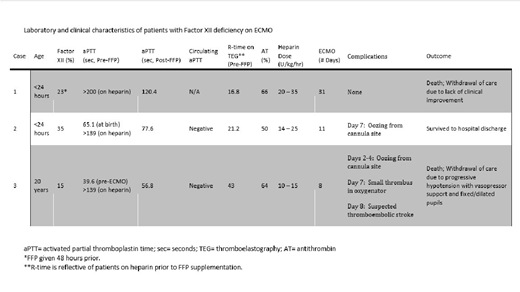
Background: Extracorporeal membrane oxygenation (ECMO) for cardiopulmonary support of critically ill patients is used frequently in the pediatric and adult population. Although a lifesaving modality, it is burdened with high morbidity and mortality as a result of hematologic complications (Dalton, et al. Am J Respir Crit Care Med. 2017). Bleeding and thrombosis are related to contact of blood and its cellular components with the non-biologic surface of the extracorporeal circuit used that results in a massive inflammatory and clotting response. Factor XII deficiency is not associated with bleeding, but results in a significant prolongation of conventional coagulation assays making them unreliable for monitoring. Here we discuss 3 cases of Factor XII deficiency and the implications it has on monitoring anticoagulation in patients on ECMO. Laboratory characteristics for all 3 patients are outlined in Table 1.
Case 1: Newborn full-term male with persistent pulmonary hypertension (PPHN) and meconium aspiration syndrome (MAS) with respiratory failure was placed on ECMO support on day of life 1. Patient received several units of cryoprecipitate and fresh frozen plasma (FFP) to correct deficiencies throughout his 31 day ECMO course. Patient did not have any bleeding or thrombotic complications, however he showed no improvement in lung function and decision was made to discontinue ECMO support.
Case 2: Newborn full-term male with severe hypoxic ischemic encephalopathy (HIE) and MAS with secondary PPHN required ECMO support on day of life 1. His Factor XII level normalized with replacement by FFP and was decannulated after 11 days of ECMO support. This patient was discharged home with family in stable condition at 5 weeks of age.
Case 3: 20-year-old female with history of recurrent astrocytoma, chronic lung disease, hydrocephalus with ventriculoperitoneal (VP) shunt, and tracheostomy presented with multifocal pneumonia and suspected sepsis. Despite fluid resuscitation and ventilatory management patient continued to have hypotension and hypoxia and thus was placed on ECMO. Prior to cannulation, patient was noted to have a coagulopathy. In addition, Factor II was low at 57% and corrected with one unit of FFP; which was thought to be related to consumptive process. On ECMO day 8, she had worsening hypotension despite vasopressor support and fixed and dilated pupils; suspected to have thromboembolic stroke and thus decision was made to withdraw life support.
Discussion: Adequate anticoagulation in patients with Factor XII deficiency requiring ECMO support presents a challenging task. Patients with Factor XII deficiency generally do not show symptoms of a bleeding disorder, which may lead to misinterpretation of coagulation assays (Kokoye, et al. Thromb Res 2016). Increased contact activation inside the ECMO cannula causes activation of platelets, consumption of Factor XII, and formation of FXIIa-antithrombin complexes that may contribute to increased risk for thrombus formation (Kokoye, et al. Thromb Res 2016 and Bachler, et al. J Thromb Thrombolysis 2019). All patients had Factor XII levels <40% on initial testing, which is sufficient to cause severe changes to the aPTT. A circulating anticoagulant aPTT was completed to assess for presence of lupus anticoagulants in 2 of the patients, which has been known to falsely elevate the aPTT and was negative (Bachler, et al. J Thromb Thrombolysis 2019). All patients received FFP in an attempt to correct deficiency and facilitate the use of aPTT and ACTs for monitoring. However, this did not prove to be successful in 2/3 patients despite receiving adult plasma. Hepzyme TEGs showed improvement in R-time post-FFP in 2 patients, but in 1 there remained evidence of factor deficiency. It is clear that traditional coagulation assays, including aPTT and ACT, become unreliable and the R-time on TEG becomes difficult to dissect heparin versus coagulation factor effect. We recommend attempting to correct factor deficiency with FFP to potentially decrease risk of thrombotic complications, and choosing an alternative laboratory monitoring assay for heparin, such as Anti-Xa levels, which may more accurately correspond to the anticoagulation status in this population. Currently, we are running a modified thrombin generation assay in these Factor XII deficient patients, pre/post-FFP, to identify if there is a decrease in thrombin generation post-FXII/FFP supplementation.
Chitlur:Bayer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda/Shire: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bioveritiv/Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees; CSL-Behring: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios: Research Funding; Octapharma: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novo Nordisk Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.