Introduction
In the last decades, survival outcomes tremendously improved in acute promyelocytic leukemia (APL) due to all‐trans retinoic acid (ATRA)/anthracycline‐based chemotherapy, and more recently ATRA/arsenic trioxide (ATO) combinations. Despite the excellent results, with response rates exceeding 90%, early death (ED), mainly due to hemorrhagic complications occurring during the first 30 days after diagnosis, remains an unsolved issue. The prevalence of ED is largely underestimated due to discrepancies between data deriving from clinical trials, reporting 3-10% rates, and real-life, where it ranges from 10 to 30% of cases, and still remains the dominant cause of poor outcome. The most common site of bleeding is the brain (65%), particularly in fatal cases. Many theories have been proposed to elucidate the pathophysiology of this complication, considering the coagulopathy of APL and the perturbed homeostasis as primum movens, but no specific neuroradiologic studies have been conducted so far. Moreover, there is no specific predictor for bleeding events in APL, with exception of increased white blood cell counts (WBC).
Patient and Methods
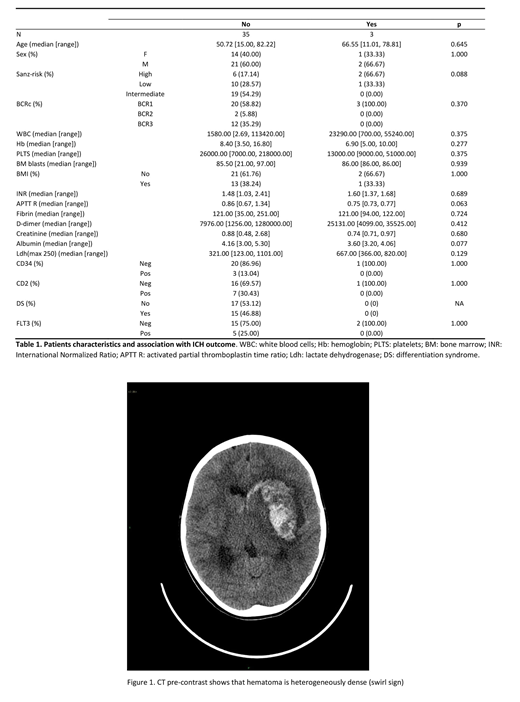
We retrospectively identified 38 patients with APL (23 males and 15 females with a median age of 51.83 years, range 11-82), consecutively diagnosed at our Institution between 2004 and 2019, and treated with standard ATRA-based induction (Table 1). Occurrence of ED and ICH was then correlated with clinico-biological parameters, selecting for commonly reported variables predictors of these complications. In addition, CT scans of the 5 patients who experienced an intracranial hemorrhage (ICH) were revised by an expert neuroradiologist, looking for radiographic predictors of poor outcome (Al-Mufti et al 2018).
Results
Approximately 13% (5/38) of our APL patients experienced an ICH during induction therapy, which was fatal in 3 cases, while the overall incidence of ED was about 10% (4/38, including 1 case of death due to a differentiation syndrome). Looking at clinico-biological variables, the only predictor of ICH was a lower albumin level at baseline (3.8 vs 4.2 gr/dl; p=0.022), as compared to patients who did not experience ICH. A high Sanz-risk score was present in 2 of 3 pts with a fatal outcome of ICH (67% of cases), together with a shorter activated partial thromboplastin time (aPTT, 0.75 vs 0.86 ratio)(Table 1). Looking at neuroradiological findings (Figure 1) the three fatal cases showed a wider ICH volume, with perilesional edema and, interestingly, a positive "swirl" sign, which is defined as a marker of ongoing extravasation of blood within a hematoma. Both cases with a favourable outcome had a cerebellar involvement, without perilesional edema, and no major involvement of basal ganglia or thalamus. None of the patients had radiological signs of arteriovenous malformations.
Conclusions
Our data remark the impact of lower albumin levels at baseline and of a high Sanz-risk category on ED in patients with APL. In APL cases with fatal ICH, the thrombo-hemorrhagic imbalance is more profound than in other AMLs and results in a more devastating clinical picture. Taking into account the limitations of the small sample size, we found that a wide hemorrhage volume with perilesional edema, and the presence of the "swirl" sign are characteristic of fatal cases, while arteriovenous malformations did not seem to play a predisposing role. Further studies including large series of patients are warranted to identify the characteristics and the possible strategies to ameliorate the outcome of ICH in APL.
Venditti:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy; Astellas: Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees; Daiichi-Sankyo: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.