Introduction
Isocitrate dehydrogenase (IDH) mutations are present in up to 20% of acute myeloid leukemia (AML) patients and lead to production of 2-hydroxyglutarate which promotes impaired differentiation and leukemic cell proliferation. Currently, there are two FDA-approved IDH inhibitors for the treatment of AML: enasidenib and ivosidenib. It is now imperative to establish timely testing so that patients can take advantage of these new therapies. Here we compared three different genotyping strategies to identify the most reliable and cost-effective way of picking up IDH1 and IDH2 mutations in AML.
Methodology
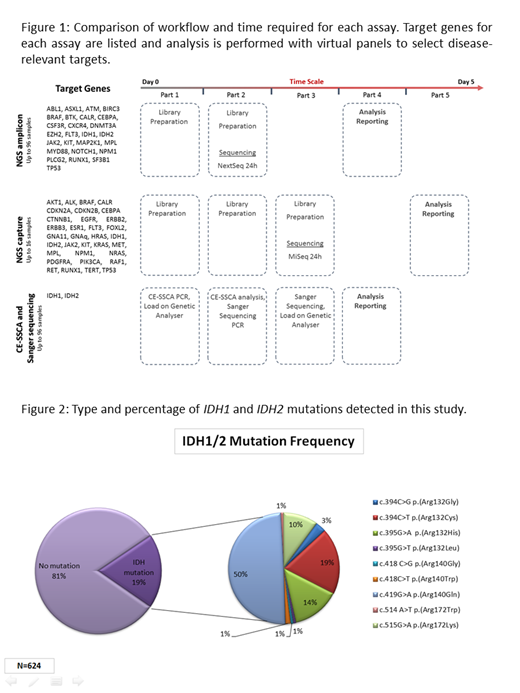
We have tested 60 AML patient samples across three different methods for detection of IDH1/2 mutations: (i) Capillary Electrophoresis-Single Strand Conformational Analysis (CE-SSCA) with Sanger sequencing, (ii) Next generation sequencing (NGS) myeloid capture panel (SureSeq myPanel, Oxford Gene Technology, OGT; UK) and (iii) multi-cancer NGS amplicon panel (QIAseq Targeted DNA Panel, Qiagen, Germany). The NGS capture assay is a 26 gene panel designed for myeloid-related genes while the NGS amplicon panel includes 33 genes associated with haematological and non-haematological malignancies (Figure 1). We have compared the techniques and assessed the quality of the results by measuring gene coverage, read depth across the panels, sensitivity and specificity per test, and performed a final valuation including some practical considerations: cost analysis, staff timings, ease of assay operation, turnaround times (TATs), ease of analysis and reporting as well as batch size limits. We initially tested 424 AML cases with CE-SSCA and have successfully transferred to amplicon panel testing (to date 200 cases).
Results
The results from the initial 60 cases were concordant between both NGS technologies and Sanger sequencing. In total across all 3 assays, we have detected IDH mutations in 19% of the 624 samples tested (Figure 2). Two samples showed false positive results by CE-SSCA, but these were identified by Sanger sequencing; therefore CE-SSCA alone is an inadequate test and all positive samples by CE-SSCA have to be confirmed by Sanger sequencing. Two samples showed IDH1 R132H mutation with variant allele frequency less than 10%, which was detected by all methods, however the Sanger sequencing trace was very small and could potentially have been missed. The gene minimum read depth for capture NGS was 682 and 677 for amplicon, and the gene mean depth was 1571 and 934 reads, respectively. We did not identify any new genetic variants in IDH1/2.
The cost of reagents was higher for the NGS capture panel at $235 per patient compared to amplicon based at $86 per patient, with CE-SSCA/Sanger sequencing combined costing $50. The amplicon NGS allows processing of up to 96 samples per batch, allowing for high throughput testing, while capture NGS only allows for 16 samples to be processed. The library preparation time (Figure 1) is shorter for NGS amplicon (2 days; 12 hours staff time) compared to capture (3 days; 17 hours staff time), with both techniques taking longer to set-up when compared to CE-SSCA (2 hours) and Sanger sequencing (1 day; 6 hours staff time). Looking at assay operation, CE-SSCA and Sanger are the less complex assays allowing for laboratory accessibility, whereas although NGS amplicon was relatively straight forward, NGS capture was slightly more complex, lending itself to specialist laboratory setup. When looking at analysis, CE-SSCA was straightforward; however certain patterns that are very similar to positive controls can lead to false positives. Both NGS analysis were very straightforward, taking <5min per sample, while CE-SSCA/Sanger can take up to 10min per sample in more difficult cases. Importantly, NGS-based approaches incorporate other clinically-relevant genes whereas CE-SSCA is limited to IDH1/2 evaluation with additional testing being required for other targets.
Conclusion:
We have established a multi-cancer NGS amplicon assay for the detection of IDH mutations in AML patients. It reduces test costs for patients, improving testing efficiencies, allowing additional clinically-relevant genes to be analysed in parallel It has also helped streamline testing for different cancer types which can now all follow the same workflow and be automated thus improving TAT's contributing to better patient management.
Acknowledgements:Celgene provided funding for this study.
Taussig:Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.