INTRODUCTION: CD19-directed chimeric antigen receptor (CAR) T cell therapy can lead to long-term remissions in a subset of patients with diffuse large B cell lymphoma (DLBCL). However, most patients fail to respond durably, and resistance mechanisms are incompletely defined. Additionally, the relative efficacy of CAR T cell therapy across DLBCL subtypes, such as T-cell/histocyte-rich large B cell lymphoma (T/HRLBCL), is not well established. T/HRLBCL is a distinct variant of large B cell lymphoma characterized histologically by rare malignant B cells scattered amongst infiltrating macrophages and reactive, yet ineffective, T cells. T/HRLBCL tumors frequently harbor genetic amplification of programmed death-ligand 1 (PD-L1) and exhibit robust infiltration by PD-L1-expressing macrophages (Chapuy et al. PMID 2971308, Griffin et al. ASH Abstract 1579, 2018). These features signify an adaptive up-regulation of the PD-L1 pathway, a negative regulator of T cell function. We hypothesized that T/HRLBCL is intrinsically resistant to CAR T cell therapy due to an immunosuppressive tumor microenvironment characterized by high expression of PD-L1 and abundant tumor-associated macrophages. Accordingly, we report 4 consecutive cases of multiply relapsed T/HRLBCL that failed to respond to CD19-directed CAR T cell therapy.
METHODS: We identified 4 patients with histologically confirmed primary-refractory T/HRLBCL who were treated with axicabtagene ciloleucel (axi-cel) CAR T cell therapy at our institution according to the FDA dose and schedule. Radiographic follow up was performed by PET/CT imaging at 30 days post-treatment. Tissue specimens were obtained at the time of clinical and radiographic disease progression to confirm persistent disease and to assess the immune context of T/HRLBCL. A fluorescence in-situ hybridization (FISH) assay was used to assess for copy number gains of chromosomal region 9p24.1, containing the PD-L1 and PD-L2 genes. To characterize the tumor-microenvironment in the setting of CAR T cell therapy resistance, multiplex immunofluorescence analysis of baseline and post-progression tumor biopsies, when available, were performed to characterize the immune infiltrate and to evaluate for PD-L1 expression by tumor cells and tumor associated-macrophages.
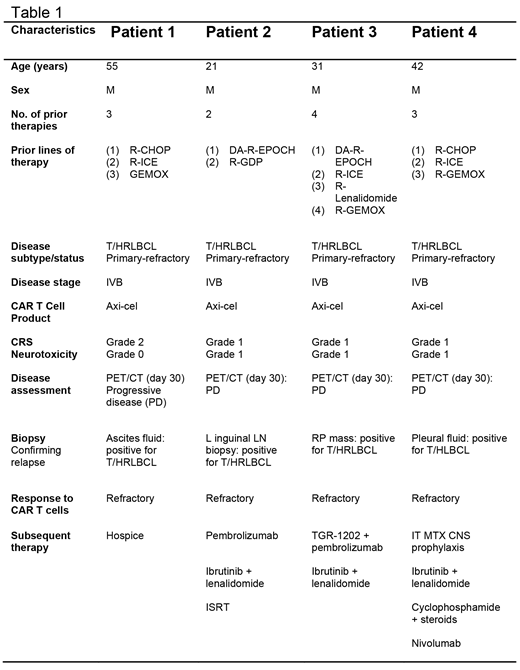
RESULTS: All the patients had primary-refractory T/HRLBCL and had received 2-4 prior lines of therapy before undergoing CAR T cell treatment (Table 1). At 30 days post-axi-cel infusion, all the patients demonstrated progressive disease. Tissue specimens obtained at the time of clinical and radiographic disease progression confirmed persistent lymphoma in all patients. In patients from whom tumor tissue is available, FISH testing for PD-L1 gene alterations, as well as, multiplex immunofluorescence analysis is ongoing and will be reported at the meeting.
CONCLUSION: Though small patient numbers, our case series suggests that axi-cel therapy may have limited efficacy in T/HRLBCL. The reasons for this are not entirely clear, though, may be related to the genetic amplification of PD-L1 and robust infiltration by tumor-associated macrophages. A prospective evaluation of disease response to CAR T cell therapy in T/HRLBCL warrants further study.
Bishop:Juno: Consultancy, Membership on an entity's Board of Directors or advisory committees; CRISPR Therapeutics: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Kite: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Riedell:Bayer: Honoraria, Speakers Bureau; Kite/Gilead: Honoraria, Research Funding, Speakers Bureau; Novartis: Research Funding; Verastem: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding. Kline:Merck: Research Funding; Merck: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract