Introduction:
Philadephia-negative Myeloproliferative neoplasms (MPNs) include polycythemia Vera (PV), essential thrombocythemia (ET) and primary myelofibrosis (PMF). The diagnosis of MPNs and further sub classification are based mainly on WHO diagnostic criteria which rely on the presence of an evidence of single or multiple cell lineage proliferation reflected by elevated hemoglobin, and / leukocytosis and /thrombocytosis. In addition, to presence of certain pathologic features in the bone marrow (BM) including hypercellularity , panmyelosis, proliferation of megakaryocytes, the presence of atypical megakaryocytes and or increased marrow fibrosis. This is in addition to the presence of molecular genetic marker specific for MPN including JAK-2, MPL and CALR. Making a diagnosis of MPN in absence of the previously mentioned features is always challenging.
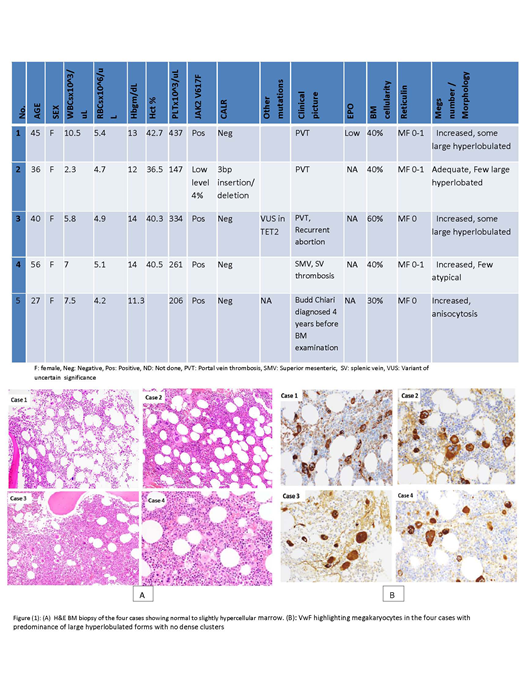
Herein, we analyze the clinical, pathologic and molecular genetics features for five cases presented with splanchnic vein thrombosis and found to be positive for JAK-2 V617F. However, from the hematpathologic point of view, apart from JAK-2 positivity, none of these cases had fulfilled the WHO diagnostic criteria for MPNs. Although the BM specimens were reviewed by at least two experienced hematopathologists, it was so difficult to conclude the diagnosis and or do further sub classification into a specific MPN category.
Objective:
The aim of this report is to highpoint the difficulty in establishing the diagnosis within this group of patients based on the current WHO diagnostic criteria, to focus on BM pathologic features of this group of patients.
Patients and Methods:
The patients reported here were referred to our center presenting with portal vein, superior mesenteric or splenic vein thrombosis. Five adult female patients were recognized (2015 and 2019). The mean age at diagnosis is 40.8 years (27-56).
None of these cases had an increase in peripheral blood counts except for patient (1) which had mild leukocytosis and thrombocytosis.
All patients showed normocellular or slightly hypercellular BM. Slight erythroid predominance was reported in patient (2) and (4). Megakaryocytes were increased in all patients except for patient (2). Interestingly, megakaryocytes morphology was similar in all five patients as they showed anisocytosis with some degree of pleomorphism with predominant of large forms, no clustering and no abnormal topography was noted (figure 1 and 2). All patients showed no significant increase in reticulin fibrosis. Sub-classification into a specific MPN category cannot be performed in all patients. Next generation sequence had been used to analyze targeted regions in recurrently mutated genes in myeloid neoplasia. JAK-2V617F mutation was detected in all studied patients. In patient number (2) JAK-2 mutation was detected at a low level (4%), however, on follow-up, the mutation level increased in addition to detection of 3bp insertion/deletion in CALR gene resulting in a mutation other than type I or type II. table (1).
Discussion:
Splanchnic veins thrombosis (SVT) includes the portal vein thrombosis (PVT), mesenteric (MVT) splenic vein thrombosis, and the Budd Chiari syndrome (BCS). SVTs are rare events, estimated by 0.7 per 100,000 patients per year for PVT [Rajani et al. 2010].
In a laboratory setting, the diagnosis of latent MPN in patients with SVT is challenging due to absence of elevated blood counts, probably caused by portal hypertension and splenomegaly that result from SVT and MPN.
However, the reason why this group of patients does not have overt features of myeloproliferation (particularly) the hypercellularity in the BM is not yet clear. It is possible that JAK-2 positivity induced venous thrombosis longer time before development of the full blown picture of MPN. However, follow-up BM studies for this group of patients might help in better characterization of the pathologic features of these patients.
These patients are included in the MPN, unclassifiable subcategory in the current WHO classification. However, based on our findings and the previously published data it seems that these patients have distinctive clinical and pathological features that necessitate having them in a separate MPN entity that might have less strict diagnostic criteria that might include clinical symptoms especially venous thrombosis in large vessels. Separating this group of patients will help to study them thoroughly.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.