Sex determination in Homo sapiens is generally dependent on the inheritance of sex chromosome combination of XX (♀) or XY (♂). One could surmise that clinical manifestations may also be sex-dependent and detectable by genetic testing. Therefore, this laboratory examined whether different cytogenetic and FISH results occur that are sex-dependent in multiple myeloma (MM) patients.
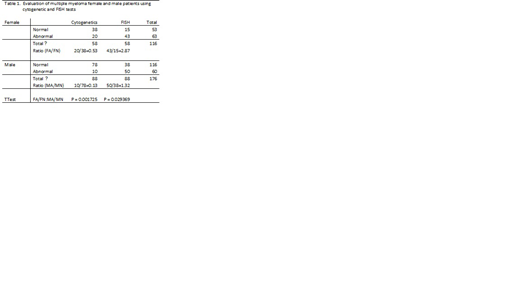
De-identified cytogenetic and FISH records of 146 MM patients (03/03/17 to 04/19/19) were retrospectively reviewed. There were 58 females (age range 40 to 88 years) and 88 males (age range of 38 to 90 years) in this survey. Data was collected from these cases and formatted into an Excel spreadsheet in order to use the TTest for statistical analyses.
Cytogenetic studies showed an abnormal-to-normal (A:N) ratio of 20:38 (0.53) in females and an A:N ratio of 10:78 (0.13) in males. This ratio for females was significantly higher than for males (P=0.003244). By FISH studies the A:N ratio was 43:15 (2.87) in females, while in males it was 50:38 (1.32) and again significantly higher in females (P=0.023312). The number of females tested was considerably less than for males (58:88=0.66), however the detection rate of abnormalities was much higher in females by both these testing methods. Specific numerical (+1 & -13) and structural abnormalities (1p & 17p modifications) detected by cytogenetics showed over-representation in females than in males. Also, FISH studies indicated that +1q and +7 were noticeably higher in females. With the exception of +7, these are genetic markers associated with poor clinical outcomes. These results are different than expected for equal distribution of abnormalities between the two genders.
The data collected showed that: 1) there are fewer females tested than males (either a true prevalence or underdiagnosed MM females), 2) the frequency of abnormalities detected by cytogenetics and FISH is higher in females than in males especially for certain markers, and 3) the 1p and -13/13q- (cytogenetics) and +1q abnormalities (FISH) found in females (but not as high in males) is not only different but may be more consequential clinically. These data suggest that there are fewer "XX" MM females (or perhaps underdiagnosed) with a higher risk of a more serious clinical outcome. By contrast, there are a greater number of "XY" MM males with a less frequent severe phenotype. MM is a multifactorial clinical entity that presently eludes a complete understanding. However, the genetic basis for MM includes sex chromosome influences that manifest chromosome abnormalities differently in females than in males.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.