Background:
Lymphoepithelioma-like carcinoma (LELC) is a rare high-grade carcinoma that can occur throughout the body. It is usually associated with Epstein-Barr virus (EBV) infection in patients from Asian countries. Pulmonary LELC occurs mostly in Asian women,, in their fifth or sixth decade, with no previous history of smoking. Optimal treatment has not been clearly established. Treatment options are based on surgery for early stage and on multimodal therapy for advanced stages.There is no report on children treated with programmed cell death 1 (PD1) inhibitor.
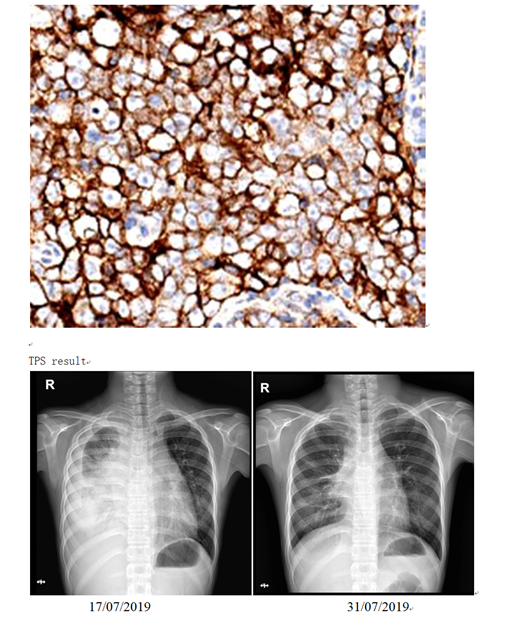
Case Description: Case 1, a 12-year-old female who was admitted for cough and serious neck swelling. PET-CT showed multiple lymph nodes enlargement in the whole body ;among them, the anterior mediastinal lesions were fused with each other and the boundary between adjacent large vessels was unclear; multiple lung and pleural metastasis . EB virus in blood was 7.48×104copies/mL.Bone marrow morphology: Naive lymphocytes account for 2.5%, some lymphocytes are irregular; Mature plasma cells easy to see.Bone marrow immunotypes: 0.56% CD19-CD5-CD10-abnormally mature B lymphocytes. Biopsy: (left neck lump) LELC, EBERs(+).Partial remission was achieved after 2 courses of paclitaxel / carboplatin/ apatinib protocal. Due to delay with varicella, the tumor came back. After the third course of treatment,she showed chest tightness and pleural effusion, EB virus in blood increased, PDL1 protein was TPS 80% positive. After one PD1 antibody combined with chemotherapy,lymph nodes and thoracic lesions significantly reduced (Image1-3), blood EB virus turned to negative. She is now continuing with PD1 inhibitor.
Case 2 , 10-year-old boy with huge right mouth bottom and right neck mass was diagnosed as LELC with EBER(+), TP53 (3%, +), CMYC (80% +). After chemotherapy, surgery and radiotherapy,he achieved complete remission.
However, multiple metastases in mediastinum lymph nodes, pleura and lung happened and surgery, chemotherapy followed by automatic stem cell transplantation and pulmonary radiotherapy were given. CT-led puncture biopsy of suspected pulmonary residual lesion showed chronic inflammation with the mild growth of the alveoli, no malignant tumor.The child took oral Tegafur as maintenance regimen. 2 months later, recurrence appeared in lymph nodes, lung ,pleural and acetabular with positive EB virus in pleural effusion. Gene detection with NGS, which includes 312 gene-wide exon region, 208 gene hotspots and 16 fusion genes, did not show mutations such as gene mutations, amplification, and fusion with a clear clinical correlation. Tumor mutation load (TMB) was low, however,the boy had attained good response after PD1 antibody followed by rescue regimen and negative blood EB virus .The 2 patients didn't develop side effects correlating with PD1 inhibitor.
Conclusion: To our knowledge, this is the first report of the use of PD1 inhibitor in children with metastatic LELC. These 2 refractory cases were all Epstein-Barr virus (EBV)-driven LELC,are more likely to respond to PD-1 blockade regardless of PD1 expresssion or TMB. EB virus burden disappeared after PD1 blockade,which perhaps can explain the anti-tumor effect.More cases are needed to verify the potential benefits of PD1 inhibitors to treat refractory LELC in children.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.