Background
Mutated cancer genes in patients (pts) with TKI failure and blast crisis (BC) CML have recently been described. RUNX1 mutations, namely single nucleotide variants (SNVs) and indels, were the most frequently detected besides BCR-ABL1 [reviewed in Branford, Kim Leuk 2019]. They were found in ~18% of pts, although splice variants were rarely described. RNA splicing events were associated with focal deletion of IKZF1 and RUNX1 in TKI resistant pts that were identified by copy number analysis and RNAseq [Branford Blood 2018]. Novel splicing associated with mutation of cancer genes is an unexplored area of study in resistance. RNA sequencing can assess the functional effect of splice site variants, which lead to splicing errors due to the use of alternative or cryptic splice sites and cause alterations to protein function.
Aim
We determined whether novel splicing can identify cancer genes with potential altered function.
Methods
RNAseq analysis was performed for 48 pts at diagnosis and 33 at BC using a protocol that preserved intron-retaining precursor RNA. Coverage of intron-exon borders was sufficient to detect intronic splice region variants. The STAR aligner was used to bioinformatically collate unannotated RNA splice junctions. 54 cancer genes were assessed and aberrant splice events were filtered based on the number of samples in which a splice junction occurred. Manual inspection of the splice junctions was performed using the Integrative Genomics Viewer. This approach identified previously verified aberrant splicing associated with IKZF1 and RUNX1 deletions.
Results
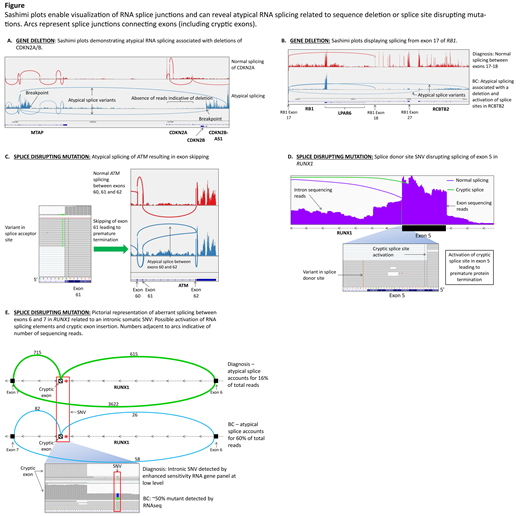
Ten previously undetected novel splice junctions were revealed in 9/33 pts (27%) in BC within key tumor suppressor genes CDKN2A/B (5), RB1 (1), ATM (1), and RUNX1 (3).
The aberrant splicing pattern of CDKN2A and RB1 (Fig A/B) in 6 pts suggested large deletions, as previously described in our cohort with IKZF1 and RUNX1 deletions. Breakpoints associated with deletions ranging from 53 to 181 Kb were detected in the 5 pts with CDKN2A aberrant splicing. Similarly, a 90 Kb deletion of exons 18-27 of the RB1 gene led to the aberrant splicing. The pts transformed to lymphoid BC (median 5 months). 4 of these 6 pts were tested at diagnosis and the deletions were not detected, indicating they were gained at resistance.
The aberrant splicing patterns of ATM and RUNX1 did not predict large deletions. These were related to somatic SNVs at canonical splice sites in ATM and in 2 of the pts with RUNX1 aberrant splicing. A splice acceptor site SNV in ATM resulted in skipping of exon 61 (Fig C) and protein truncation. This novel SNV has not been reported in any population or somatic variant database.
Two pts in myeloid BC at 28 and 48 months after diagnosis had an identical somatic RUNX1 mutation at the canonical splice donor site of exon 5. The SNV was not detectable prior to imatinib treatment in both pts. The splice site SNV led to activation of a cryptic splice site within exon 5 in both pts (Fig D), which predicted premature termination. While this mutation is novel, an adjacent intronic SNV occurs in familial platelet disorder, leading to activation of the same cryptic splice site.
The atypical RUNX1 splicing of the 3rd patient was associated with retention of 55 bp of intron 6 as a cryptic exon (Fig E), leading to protein truncation. A deep intronic SNV identified at lymphoid BC at 6 months of imatinib was detected near the cryptic exon by RNAseq and verified as somatic by DNA Sanger sequencing. This was predicted to activate cryptic RNA splicing elements and lead to intron sequence retention in a RUNX1 transcript. We sequenced the diagnosis sample using an RNA-based gene panel method under development that provides enhanced sensitivity of variant detection. The same pattern of atypical splicing was observed and the intronic SNV was present at low level. The RUNX1 mutation at diagnosis may have contributed to early BC. To our knowledge this is the first report of a RUNX1 truncating variant in CML involving a cryptic exon.
Conclusion
Enhanced bioinformatic analysis of RNAseq data has revealed a high proportion of pts with truncating mutations in cancer genes indicated by novel RNA splicing (27% pts in BC). Using RNA-based sequencing allows an evaluation of the potential functional effect of variants that are not apparent by DNA-based mutation analysis. We suggest that future studies include RNA sequencing to detect a broader spectrum of mutations associated with TKI resistance.
Shanmuganathan:Gilead: Other: Travel Support; Janssen: Other: Travel Support; Amgen: Other: Travel Support; Bristol-Myers Squibb: Honoraria, Other: Travel Support; Novartis: Honoraria, Other: Travel Support. Yeung:Novartis: Honoraria, Research Funding; BMS: Honoraria, Research Funding; Pfizer: Honoraria; Amgen: Honoraria. Scott:Celgene: Honoraria. Hughes:Novartis, Bristol-Myers Squibb, Celgene: Research Funding; Novartis, Bristol-Myers Squibb: Consultancy, Other: Travel. Branford:Cepheid: Consultancy, Honoraria; Qiagen: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding, Speakers Bureau; Bristol-Myers Squibb: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.