Background: Anemia remains one cardinal symptom associated with reduced quality of life (QoL) in patients (pts) with myelofibrosis (MF) which is normally not being addressed by ruxolitinib (RUX). In our previous MPNSG-0109 trial, single-agent pomalidomide (POM) improved cytopenia in 14% (POM 0.5 mg QD) and 29% (POM 2.0 mg QD) of MF pts, respectively. In the MPNSG-0212 study, we sought to investigate the potential synergism of RUX plus POM to improve anemia and QoL in MF pts.
Study Design: MPNSG-0212 is an ongoing multicenter, open-label, single-arm phase-Ib/II trial with a target population of 90 pts following a two-stage design (NCT01644110). Pts 1-40 in cohort 1 (co1) were treated with RUX (10 mg BID) plus low-dose POM (0.5 mg QD), while pts 41-90 in cohort 2 (co2) receive a step-wise dose increase of POM from 0.5 mg to 1 mg and 2 mg QD after 3 and 6 28-day-cycles, respectively. Primary endpoints are safety of the combination therapy, anemia response after 12 cycles (according to IWG-MRT and RBC transfusion independence [RBC-TI] criteria), and clinical benefit (CB) defined as stable disease plus i) hemoglobin (Hb) increase ≥1 g/dL in pts with RBC-TI or ii) doubling of RBC transfusion intervals and/or iii) significant (>25%) improvement of QoL as measured by the MPN-SAF questionnaire. Main inclusion criterion is MF with anemia (Hb <10 g/dL and/or RBC transfusion dependence [RBC-TD]). Pts suitable for allogeneic transplantation and pts with low platelet counts (<100/nL) are excluded.
Results: At data cut-off (31-May-2019), 79 pts were included. Data from 67 pts were available for evaluation (co1, n=40; co2, n=27). Baseline characteristics of the pts were as follows: median age 72 years (range 49-84), prior treatment in 53% (RUX in 22%, POM in 4%), median Hb level at study start 8.6 g/dL (range 5.4-11.7), RBC-TD in 28%, median spleen diameter measured by ultrasound 17.7 cm (range 12-36), presence of constitutional symptoms in 76%, and 91% intermediate-2 (61%) or high-risk (30%) pts according to DIPSS; 55% of pts in co1 had ≥1 high molecular risk mutation (ASXL1, SRSF2, EZH2, and/or IDH1/2).
Median number of cycles until data cut-off was 12 (range 2-63) in co1 and 11 (range 2-21) in co2. In total, 502 adverse events (AE) mainly grade 1/2 were recorded: AE grade 1/2 in >20% of pts were fatigue (in 27% of pts), dyspnea (24%), diarrhea (22%), and muscle cramps (21%); AE grade ≥3 in >3% of pts was Hb decrease in the first weeks of treatment occurring in 25% of pts. In total, 87 serious AE (SAE), were recorded: most common SAE (in ≥3 pts) were pneumonia (in 15% of pts), leukemic transformation (9%), worsening of general condition (6%), CNS ischemia, and sepsis (4% each); 7 SAE (in 10% of pts) were grade 5.
Number or severity of (S)AE was not increased in co2. Treatment interruptions of RUX and/or POM were necessary in 11 pts (27%) of co1 and 3 pts (11%) of co2; 2 pts stopped treatment permanently due to hematotoxicity. Increase of the POM dose to 1 mg and 2 mg QD was feasible in the majority of pts after 3 and 6 cycles, respectively.
In co1, 18/40 pts (45%) continued treatment beyond cycle 12 because of an objective anemia response (7/40, 18%: clinical improvement [CI, Hb increase ≥2 g/dL] n=5, partial remission and RBC-TI n=1 each) or CB (11/40, 27%): Hb increase ≥1 g/dL and/or doubling of RBC transfusion intervals (n=4) or improvement of QoL according to MPN-SAF (n=7). In co2, 17/27 pts (63%) reached cycle 12 and 10/17 (59%) continued treatment: 2/10 (20%) experienced CI, whereas 8/10 (80%) fulfilled the CB criterion; 19/27 pts (70%) were still on treatment at the time of data cut-off.
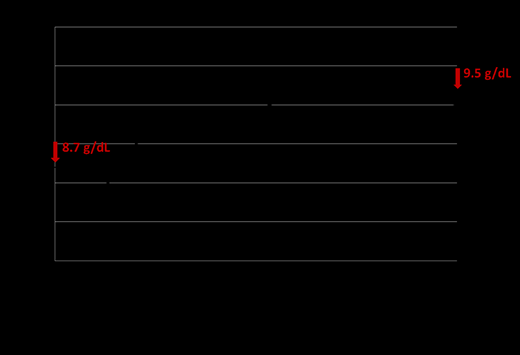
Among all 67 pts analyzed, 42% (28/67) were on treatment for more than 12 cycles and 24% (16/67) for more than 24 cycles; 3 pts (4%) were treated for more than 60 cycles due to sustained response or CB. Of note, mean Hb increased from 8.7 g/dL at baseline to 9.6 g/dL at end of cycle 18 and remained stable thereafter (Figure 1).
Conclusions: Combination treatment using RUX plus POM is feasible in pts with poor-risk MF and resulted in an objective anemia response rate of 18% in co1. Of note, 42% of pts were treated with >12 cycles and showed a longer lasting stabilization of their disease with sustained improvement of Hb and QoL. Step-wise increase of the POM dose in co2 is safe and feasible with 70% of pts still on study treatment. Updated efficacy results of co2 with longer follow-up data will be presented at the meeting.
Stegelmann:Incyte: Consultancy, Honoraria; Novartis: Consultancy, Honoraria. Koschmieder:Pfizer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Bristol Myers-Squibb: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis Foundation: Research Funding; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Incyte: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Ariad: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; AOP Pharma: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; CTI: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Shire: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Isfort:Novartis: Consultancy, Honoraria, Other: Travel reimbursement; Pfizer: Consultancy, Honoraria, Other: Travel reimbursement; Ariad: Consultancy, Honoraria; BMS: Honoraria; Hexal: Other: Travel reimbursement; Amgen: Other: Travel reimbursement; Mundipharma: Other: Travel reimbursement; Roche: Other: Travel reimbursement; Alexion: Other: Travel reimbursement. Hochhaus:Pfizer: Research Funding; Novartis: Research Funding; BMS: Research Funding; Incyte: Research Funding; MSD: Research Funding. Göthert:Bristol-Myers Squibb: Consultancy, Honoraria, Other: Travel support; Incyte: Consultancy, Honoraria, Other: Travel support; Pfizer: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Other: Travel support; Proteros Biostructures: Consultancy; AOP Orphan Pharmaceuticals: Honoraria, Other: Travel support. Schafhausen:Incyte: Consultancy, Equity Ownership, Honoraria; Novartis: Consultancy, Honoraria. Radsak:Daiichi Sankyo: Other: Travel Support, Advisory Boards; Novartis: Other: Travel Support, Advisory Boards; JAZZ: Other: Travel Support; Celgene: Other: Travel Support, Advisory Boards; Takeda: Other: Advisory Boards; Otsuka: Other: Advisory Boards. von Bubnoff:Novartis: Research Funding. Reiter:Blueprint: Consultancy, Honoraria, Other: Travel reimbursement; Novartis: Consultancy, Honoraria, Other: Travel reimbursement, Research Funding; Deciphera: Consultancy, Honoraria, Other: Travel reimbursement. Döhner:Celgene, Novartis, Sunesis: Honoraria, Research Funding; AbbVie, Agios, Amgen, Astellas, Astex, Celator, Janssen, Jazz, Seattle Genetics: Consultancy, Honoraria; AROG, Bristol Myers Squibb, Pfizer: Research Funding. Griesshammer:Novartis: Consultancy, Honoraria, Speakers Bureau. Döhner:Daiichi: Honoraria; Jazz: Honoraria; Novartis: Honoraria; Celgene: Honoraria; Janssen: Honoraria; CTI Biopharma: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.