Introduction
Arterial and venous events are known to occur in patients with POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal gammopathy, Skin changes) syndrome which may also include myeloproliferation, with a reported rate in the literature of around 20%. This is higher than in the myeloma cohort where the VTE rate from the UK Myeloma XI study was reported as 11.8%. The approach to optimum management of thrombosis in POEMS patients remains undefined.
Method
The UCLH POEMS Registry is a comprehensive tertiary centre-based UK data repository including patients from 1999 to the present. Data were collated from patients referred in for diagnosis or after treatment and included blood results, neurological and general performance status, previous and active venous thromboembolism (VTE) and arterial events and their management.
Results
Of the 103 patients in the UCLH POEMS Registry, 20 were excluded due to missing data. Of the 83 patients included, median age was 52 years (31-84) and 54 (65%) were male. Mean haemoglobin at diagnosis was 143 g/L (89-190), platelet count 443 x10^9 (194-741), vascular endothelial growth factor (VEGF) 3536 pg/mL (388-15422), creatinine 75 μmol/L (32-168) and albumin 40 g/L (31-50). Performance status was ≥ 3 in 15 patients.
Radiotherapy was used as a treatment modality in 21/83 (25%) and 48/83 (52%) patients received autografts. There were 51 outpatient-based chemotherapy regimens prescribed. Lenalidomide and dexamethasone (LD) was the most common prescription 30/51 (59%), followed by cyclophosphamide and dexamethasone in 10/51 (20%), LD plus cyclophosphamide in 3/51 (6%), melphalan and steroids 3/51 (6%), cyclophosphamide, dexamethasone and thalidomide 2/51 (4%), LD plus ixazomib 1/51 (2%), velcade, thalidomide and dexamethasone 1/51 (2%) and carfilzomib with dexamethasone 1/51 (2%).
Of these 51 outpatient-based chemotherapy scripts, 30 received documented thromboprophylaxis (TP). Prophylactic low molecular weight heparin (pLMWH) was prescribed most frequently (17/30) with 16 of these patients receiving an immunomodulatory based chemotherapy regimen. Other TP agents used include: aspirin (6/30), treatment dose LMWH (tLMWH) (2/30), rivaroxaban (2/30), warfarin (2/30) and clopidogrel (1/30).
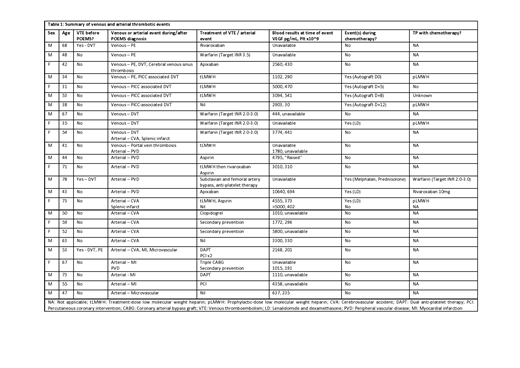
Twenty-five patients experienced a total of 35 clinically apparent arterial or venous events. Seven had more than 1 thrombotic event, 2 of which developed both arterial and venous thromboses. Three patients had a prior history of VTE;1 with historic DVT developed pulmonary emboli, and 2 had arterial events after historic VTE.
Eleven patients had 14 VTEs including DVT (6/14), PE (4/14) and 4 PICC-associated DVT occurring during melphalan-based autograft. Most VTEs occurred during active disease with median VEGF 2731 (444-5000). Five venous events occurred on chemotherapy, including 4 during a melphalan-based autograft, and 1 on LD. VTE occurred despite prophylactic LMWH in 3 patients (2 unknown). Treatment comprised LMWH (4), warfarin (4), or the direct oral anticoagulants, rivaroxaban (1) and apixaban (1). One patient did not receive treatment for a PICC-associated DVT.
Sixteen patients experienced 21 arterial events including stroke (7/21), peripheral vascular disease (6/21), MI (4/21) and microvascular disease (2/21). Most events occurred during active disease with median VEGF 3155 (637-10640). Three occurred on anti-POEMS therapy: one patient (VEGF 4555) developed a second stroke on LD and LMWH prophylaxis; one patient on LD (VEGF 10640) and prophylactic rivaroxaban 10mg developed PVD, and another on melphalan and prednisolone (VEGF 2000-4000) and warfarin for atrial fibrillation (target INR 2.0-3.0) developed PVD.
Conclusion
The venous and arterial event rate in this cohort at 35/83 (42%) is over double that previously reported. There were more arterial events than venous, and most occurred in a state of active disease and off anti-POEMS therapy (26/35), suggesting that treatment-related risk factors are less of a driver for thrombosis than the disease itself. There was no discernible relationship with thrombocytosis. Thromboprophylaxis is commonly used in POEMS patients receiving outpatient-based chemotherapy with the most common agent being prophylactic LMWH. With the high incidence of arterial events in the presence of active disease, the role for anti-platelet agents or indeed DOACs remains undefined in this patient group.
Thomas:Sanofi: Membership on an entity's Board of Directors or advisory committees. D'Sa:Janssen: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.