Introduction: Adverse health outcomes following recovery from thrombotic thrombocytopenic purpura (TTP) are under-recognized. The Oklahoma (OK) TTP Registry has documented that patients have residual complications following recovery. TTP survivors have an increased prevalence of major depression, decreased quality of life, minor cognitive impairment, and a decreased life expectancy compared to the general population. Additionally, Chaturvedi et. al (2017), reported that 32% of TTP survivors met the provisional diagnosis of post-traumatic stress disorder related to their TTP. Yet studies have failed to assess the significance of residual complications from the survivor's perspective. The goal of this study was to determine from the survivor's perspective, long-term outcomes that impact daily activities during remission.
Patients: TTP survivors were recruited from the OK Registry and the Ohio State University (OSU) TTP Research Program. Eligibility included: 1) age >18 years, 2) documented ADAMTS13 deficiency, 3) in clinical remission from TTP, and 4) able to read and understand English.
A non-probabilistic purposive sampling approach was utilized to select survivors from whom the most could be learned. To understand the full range of health challenges during remission, we intentionally included > 1 person who had experienced a TTP relapse in each focus group.
Methods: Qualitative focus groups were conducted using a semi-structured discussion guide to facilitate and standardize the discussion. Prior to use, the discussion guide was pilot-tested and revised accordingly. All the focus groups were conducted in-person and moderated by the first author.
During the focus group, TTP survivors described symptoms following recovery. All of the mentioned symptoms were transferred to index cards and given to each person. Patients individually sorted the cards into 'high', 'medium', and 'low' impact on daily living. Next, patients discussed views on what makes a symptom high, medium, or low impact. Additionally, patients were asked to list their top 3 symptoms on an index card (regardless of if it had been previously mentioned). Patients were also asked about discussions with their physicians regarding these symptoms. Frequencies were calculated for quantitative responses. Qualitative data were analyzed for themes.
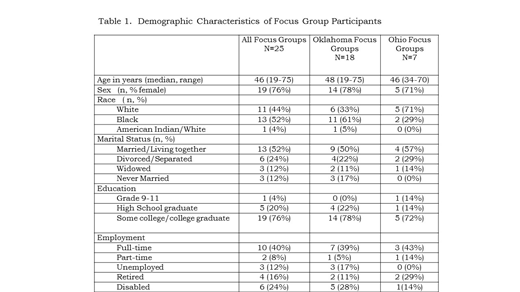
Results: Focus groups (4 in OK; 3 in OSU) were conducted from May-Oct. 2018, were 54-94 minutes, and digitally recorded. Overall, there were 25 patients (76% female, 52% black, median age 46 years) (Table 1). Eighty percent of patients were >5 years from their last episode, 52% had experienced a TTP relapse.
The top 2 symptoms listed on the cards were: cognitive impairment 19/25 (76%) and fatigue 17/25 (68%). These symptoms were ranked as high in patients who were both < and >5 years from their last episode. High-impact symptoms occurred daily and negatively affected self-esteem, relationships, and careers. In 6/7 focus groups, survivors described high-impact symptoms caused feelings of being a burden, embarrassment, depression, and anxiety. Fatigue kept survivors from activities with loved ones and the hobbies they enjoyed prior to TTP. Cognitive impairment was described as difficulty 'getting the right words out', forming complete thoughts, and problems with memory and concentration. Cognitive impairment often resulted in arguing and frustration with loved ones. In 4/7 focus groups, memory and concentration problems were detrimental to marriages/long-term relationships. In 5/7 focus groups, cognitive impairment significantly impacted a person's ability to do their job. In 1 focus group, patients who worked in healthcare stated they changed careers because they feared their memory problems would negatively impact the health of others.
Yet, many patients were hesitant to discuss these symptoms with a physician because they: 1) did not want to complain, 2) did not want to be prescribed additional medication, and 3) did not think these symptoms were relevant to their 'blood doctor'.
Conclusion: Cognitive impairment and fatigue have serious impacts on daily living even >5 years after TTP. Yet, patients were often hesitant to discuss the issues with their doctor and failed to connect these symptoms with the TTP recovery process. Phase II of this study is currently underway, the goal is to identify from the TTP survivor's perspective, preferred ways to assess and manage these symptoms.
Terrell:National Institutes of Health: Research Funding. Cataland:Alexion: Consultancy, Research Funding; Ablynx/Sanofi: Consultancy, Research Funding. Panepinto:NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.