Abstract
CD19-targeted immunotherapies have drastically improved outcomes for relapsed/refractory (r/r) B-cell acute lymphoblastic leukemia (ALL) patients. Such therapies, including blinatumomab and CD19 chimeric antigen receptor (CD19CAR) T cells, yield high remission rates and can bridge to more definitive consolidation therapy with curative intent. Both treatments are approved by the US Food and Drug Administration (FDA) for r/r ALL (CD19CAR T-cell approval is restricted to patients ≤25 years old). Although availability of blinatumomab and CD19CAR T cells has extended options for the treatment of r/r ALL, prioritizing the sequence of these agents on an individual-patient basis may be difficult for the treating physician. Considering each therapy’s advantages, limitations, and challenges is necessary when choosing between them. Although patients may receive both blinatumomab and CD19CAR T cells sequentially in cases that fail to respond or subsequently relapse, a proportion of patients treated with CD19-targeted immunotherapy will lose expression of CD19 and will be excluded from receiving the alternative CD19-targeted therapy. Thus, weighing all considerations for each patient before selecting a CD19-targeted immunotherapy is crucial. Here, we discuss real-life scenarios of adults with r/r ALL, in which we selected either blinatumomab or CD19CAR T-cell therapy, and the rationale behind each decision.
Introduction
In the preimmunotherapy era, adults diagnosed with relapsed/refractory (r/r) acute lymphoblastic leukemia (ALL) had poor prognoses,1-6 largely due to the paucity of effective salvage therapies. Since the introduction of immunotherapy, patients with B-cell ALL have a better chance of achieving remission and being bridged to a curative allogeneic hematopoietic cell transplantation (allo-HCT).
CD19 is a cell-surface protein that is expressed widely on B-cell ALL blasts. There are 2 US Food and Drug Administration (FDA)-approved immunotherapies for r/r ALL that target CD19, blinatumomab, and CD19-directed chimeric antigen receptor (CD19CAR) T cells. Blinatumomab is approved for r/r B-cell ALL, including minimal residual disease (MRD), for any age, whereas CD19CAR T cells are approved for B-cell ALL that is refractory or in second or later relapse for patients up to 25 years of age. Blinatumomab is a CD3/CD19-bispecific antibody that engages T cells with CD19+ leukemic cells creating a cytolytic synapse, which mediates leukemic cell lysis. In contrast, CD19CAR T cells are generated by transducing autologous T cells with a virus expressing a chimeric receptor that recognizes CD19. CD19CAR T cells are expanded ex vivo and infused back into the patient where they bind to and eliminate CD19+ ALL cells. Targeting CD19 has limited off-tumor targeting with tolerable consequences. Both CD19-targeted immunotherapies have produced striking responses in advanced ALL. Tables 1 and 2 describe clinical studies for blinatumomab and CD19CAR T cells for ALL.
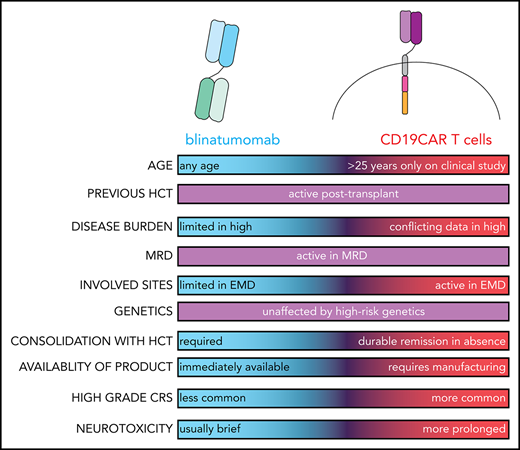
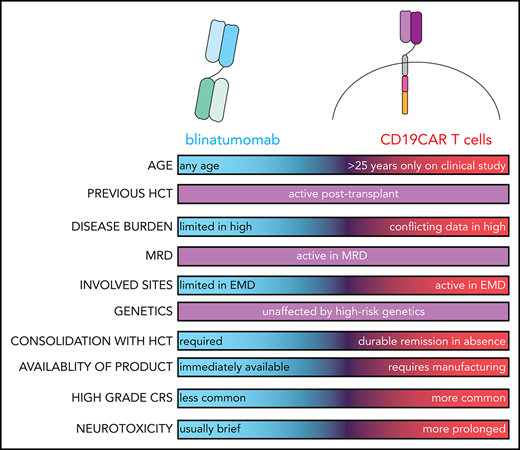
Once the decision to use CD19-targeted immunotherapy to treat a patient with advanced ALL has been made, the physician faces the challenge of selecting between blinatumomab and CAR T cells. There are advantages, limits, and challenges with each therapy that are unique for an individual patient, and it is necessary to consider factors such as age, fitness, disease burden, involved sites, T-cell product manufacturing, and availability of an allogeneic donor when choosing between these 2 options. It is sometimes feasible to deliver both therapies sequentially in cases that fail to respond or subsequently relapse following 1 treatment. However, some patients treated with CD19-targeted immunotherapy lose CD19 antigen expression at the time of treatment failure or relapse, and in selecting 1 CD19-targeted immunotherapy, it is possible that the patient subsequently may be ineligible to receive the other CD19-targeted immunotherapy. Thus, it is crucial to weigh all considerations for each individual patient before selecting one immunotherapy over another.
It is critical to highlight that both blinatumomab and CD19CAR T-cell therapy are extremely expensive. In fact, tisagenlecleucel is among the most expensive drugs ever approved for cancer treatment (∼$500 000 per single product). Likewise, 1 cycle of blinatumomab costs ∼$89 000. However, because access to these therapies is often determined by insurance coverage or by availability of clinical trials, we believe that cost may have limited influence on therapy selection. Because ALL is rare and usually affects younger patients with many years of potential productivity, studies are needed to demonstrate the cost-efficiency of these drugs, and their impact on the financial burden of the health system. Although these novel immunotherapies are approved in North America and some European countries, they are not readily available in most of the developing world, and, unfortunately, treatment of advanced ALL in these countries is restricted to traditional, less effective therapies.
Which CD19-targeted immunotherapy to select for an individual patient with ALL is an evolving question that will be informed by additional clinical studies. One such ongoing clinical study (NCT03628053) comparing tisagenlecleucel vs blinatumomab or inotuzumab in r/r ALL will address some of the considerations when selecting between the 2 therapies. Here, we discuss 5 real-life scenarios where adults with r/r ALL were treated with blinatumomab or CD19CAR T cells, and the rationale behind that treatment decision based on our current understanding of the likelihood of efficacy in these specific situations.
Patient 1: older patient with relapsed CD19+ ALL with low disease burden
Patient 1 was a 64-year-old woman diagnosed with ALL with hyperdiploidy. She achieved complete remission (CR) following induction, but her treatment was interrupted for 3 months due to necrotizing pneumonia. Upon recovery, she received maintenance therapy but relapsed within 3 months, and bone marrow (BM) biopsy revealed 10% CD19+ lymphoblasts. Her brother was known to be a full HLA match and willing donor. She was treated with blinatumomab and achieved negative MRD CR. She experienced grade 2 neurotoxicity requiring a brief course of dexamethasone. She underwent allo-HCT from a matched sibling donor (MSD), and is now 2 years posttransplant in remission with only mild chronic graft-versus-host disease (GVHD).
Outcomes of ALL in older adults (>60 years) are extremely poor. Older patients more frequently carry high-risk genetics and tolerate chemotherapy poorly, making it difficult to deliver adequate curative therapy.7-11 The lack of treatment options for older adults becomes even more pronounced in the setting of salvage therapy. Thus, incorporating novel therapies after treatment failure in older patients with ALL is crucial.
Blinatumomab is approved across all ages and can be readily provided to older patients with r/r ALL. Clinically, blinatumomab produces a comparable CR/CR with partial hematopoietic recovery (CRh) rate (56% vs 46%) and median overall survival (OS), regardless of patient age (≥65 years old or <65 years old) in advanced ALL.12 However, older patients more frequently develop high-grade neurotoxicity (28% vs 13%) compared with younger patients.12 Furthermore, favorable outcomes are observed in elderly patients (median age, 75 years) with newly diagnosed ALL treated with blinatumomab in the frontline setting, with a CR/CRh rate of 66%, and no deaths occurring in the first 4 weeks of treatment.13
CD19CAR T-cell therapy is currently only available as an investigatory drug in adults >25 years old. Although response to CD19CAR T-cell therapy in r/r ALL is astonishing in younger adults, experience with CD19CAR T-cell therapy in older adults (>60 years old) is limited. Nonetheless, 6 of 8 older adults (>60 years; 75%) with r/r ALL treated on the Memorial Sloan Kettering Cancer Center (MSKCC) study responded,14 and all 4 older patients with ALL treated on the Fred Hutchinson Cancer Research Center (FHCRC) study achieved CR.15 Thus, it is likely that age itself does not detrimentally impact response to CD19CAR T cells. However, treatment toxicity is a serious concern, given the difficulty elderly patients have in enduring severe cytokine release syndrome (CRS) and neurotoxicity, both of which occur more frequently with CD19CAR T cells compared with blinatumomab.14-17 However, expected toxicity of CAR T-cell therapy in low disease burden (eg, MRD) is low. Therefore, CAR T-cell therapy can be indicated for older patients with low disease burden.
Patient 1 had low leukemia burden in her marrow at relapse, another factor that prompted us to recommend blinatumomab. There is an inverse relationship between disease burden and response to blinatumomab in r/r ALL, with tumor burden of <50% marrow blasts correlating with higher response rate (CR/CR with incomplete hematological recovery [CRi] = 73% vs 29%).18-20 In CD19CAR T-cell studies, the definition of disease burden and impact of disease burden on efficacy both varied. In the MSKCC study, higher leukemia burden was defined as >5% marrow blasts or presence of extramedullary disease (EMD), and adversely affected CD19CAR T-cell outcomes (CR = 75% vs 95%; P = .07), with worse OS (P = .02) and event-free survival (EFS) (P = .01).14 However, investigators from Seattle Children’s Hospital observed no correlation between disease burden (classified according to marrow blasts as M1 [<5%], M2 [<25%], and M3 [≥25%]) and efficacy of CD19CAR T-cell therapy.21 As a final consideration, higher leukemia burden at the time of lymphodepletion is correlated with severe CRS during CD19CAR T-cell therapy.14,22
For this patient, our definitive curative plan included allo-HCT because she had an MSD. Thus, to expedite this patient to allo-HCT, we chose blinatumomab as it was immediately available without needing to allocate a slot on a clinical study or wait for CAR T-cell manufacturing. Other considerations included a high likelihood of response to blinatumomab considering her low disease burden at relapse and lower expected toxicity with blinatumomab compared with CD19CAR T-cell therapy in older patients.
Patient 2: extramedullary relapsed ALL
Patient 2 was a 22-year-old man with ALL. He was treated with an adolescent–young adult regimen23 and achieved MRD− CR postinduction. He experienced an isolated central nervous system (CNS) relapse early during maintenance. The CNS disease was cleared with high-dose methotrexate combined with intrathecal chemotherapy. A matched unrelated donor (MUD) was identified, however, pretransplant BM biopsy showed evidence of MRD relapse at 0.02%. Transplant was suspended and he underwent leukapheresis in preparation for CD19CAR T cells. The prelymphodepletion cerebrospinal fluid (CSF) evaluation showed evidence of lymphoblasts in the CSF (CNS-2, <5 WBC/μl CSF with lymphoblasts present) and a BM biopsy revealed ongoing persistent MRD at 0.15%. He received CD19CAR T cells (tisagenlecleucel) and exhibited low-grade CRS, which resolved after tocilizumab. Evaluation at day 28 postinfusion documented MRD− CR in the marrow and undetectable blasts in the CSF.
EMD is prevalent in relapsed ALL, with CNS involvement being common. ALL involving the CNS is challenging because most available therapies do not cross the blood-brain barrier to achieve therapeutic concentrations in the CSF. Patients with history of CNS relapse have increased risk of leukemia recurrence in the CNS even after allo-HCT.24
CD19CAR T cells can be detected in the CSF after infusion,15,21,25-27 and at higher levels in patients who develop neurotoxicity.25 Importantly, treatment with CD19CAR T cells can eradicate CSF leukemia,21,22,25 as seen for patient 2. Gardner et al reported 9 patients with lymphoblasts in the CSF prelymphodepletion who all responded to CD19CAR T cells, clearing CSF blasts.21 This propriety of CD19CAR T cells to traffic to the CNS and induce antileukemic killing has led to the inclusion of patients with CNS leukemia in many recent CD19CAR T-cell studies. In 1 study, CD19CAR T-cell therapy was administered intrathecally to 3 patients with uncontrolled CNS-relapsed ALL. Intriguingly, all patients attained remission with reversible toxicities.28 Promising antileukemic activity for CD19CAR T-cell therapy is also reported for extramedullary sites other than the CNS.15,26,27,29 For instance, 6 of 7 patients with EMD treated in the FHCRC study attained CR,15 whereas Jacoby et al reported that all cases with resistant EMD sites (n = 8) resolved after CD19CAR T-cell treatment.29
In contrast, data on blinatumomab trafficking to the CSF and other EMD sites is lacking. We have shown that history and/or presence of active EMD at the time of initiating blinatumomab predicts poor response to treatment.19 Moreover, EMD relapse following blinatumomab seems overrepresented compared with other therapies.19,30,31 Thus, blinatumomab is likely not the optimal choice for relapsed ALL with bulky EMD and/or CNS involvement. Tables 1 and 2 depict the number of cases with EMD and CNS involvement in published clinical studies for CD19-targeted immunotherapies.
In this case, our rationale for selecting CD19CAR T-cell therapy was the patient’s history of CNS relapse and our concern about future CNS recurrence even after allo-HCT, after which there would be limited therapeutic options. Current data support encouraging activity of CD19CAR T cells in eradicating CNS disease (at least in CNS-2) and potentially preventing CNS relapse. However, these data remain preliminary and require confirmation in larger studies, especially due to safety concerns about neurotoxicity associated with CD19CAR T-cell therapy in patients with active CNS involvement. Current data for blinatumomab support limited activity in ALL involving the CNS, and we observe frequent extramedullary failure during therapy, which further informed our decision to treat this patient with CAR T cells.
Patient 3: CD19+ targeting of ALL pre– and post–allo-HCT
Patient 3 was a 27-year-old man diagnosed with Philadelphia chromosome–positive ALL who achieved CR with dasatinib and steroids. He underwent allo-HCT from an MUD, but relapsed 1 year later. He achieved a second CR with chemotherapy and dasatinib, and was placed on maintenance dasatinib. He experienced a second relapse 1 year later and failed to respond to a ponatinib-based regimen. He was enrolled on a CD19CAR T-cell clinical trial (NCT02146924). His treatment course was complicated by grade 2 CRS that required tocilizumab. He achieved a third MRD− CR prior to undergoing another allo-HCT from a different MUD. He is now over 1 year postsecond allo-HCT and remains in remission.
Although failing a prior allo-HCT is associated with low response to salvage chemotherapy in ALL,1,3 it does not impact response to CD19-targeted immunotherapy. Patients with relapsed ALL with and without prior allo-HCT respond comparably to blinatumomab (CR/CRi is 45% vs 43%, respectively), demonstrating that blinatumomab activity is independent of previous allo-HCT.32-35 Likewise, response to CD19CAR T-cell therapy is remarkable in patients with r/r ALL irrespective of prior allo-HCT,14,21,22,36,37 and neither OS nor EFS was influenced by history of allo-HCT in the Children’s Hospital of Philadelphia (CHOP) experience.22 Therefore, both CD19-targeted immunotherapies are valid options for treating our patient who relapsed post–allo-HCT.
Another consideration when choosing CD19-targeted immunotherapy for ALL following allo-HCT relapse is the potential for the development of GVHD. New-onset GVHD was encountered at an alarming rate (55% of patients) and severity (high grade = 29%) in patients treated with checkpoint inhibitors following allo-HCT relapse.38 Reassuringly, the occurrence of high-grade GVHD following CD19-targeted immunotherapies in allo-HCT recipients is rare. Stein et al reported that only 7 of 64 patients (11%) with prior allo-HCT treated with blinatumomab developed GVHD, which was mostly low grade and not requiring treatment discontinuation.32 Similarly, the GVHD rate following CD19CAR T-cell therapy has been low (0% to 9%) in allo-HCT recipients.15,21,22,25,39
For ALL relapses post–allo-HCT, various factors influencing the choice of CD19-targeted immunotherapy include timing of relapse post–allo-HCT (early vs late), availability of the original donor (sibling vs unrelated) for T-cell collection, and whether the patient requires immunosuppressive therapy due to GVHD. Early relapse post–allo-HCT, especially if the patient is receiving immunosuppressive therapy or if the donor was unrelated, may impact the quality of autologous T-cell collection for CAR T-cell manufacturing. Recent or active GVHD requiring immunosuppressive therapy often precludes the use of either CD19-targeted immunotherapy, as both therapies mediate antileukemic activity via T cells, which are major players in GVHD and are inhibited by immunosuppressive therapy.
One consideration when choosing a CD19-targeted immunotherapy for patients with relapsed ALL post–allo-HCT is the possibility of a future second allo-HCT. For patients unlikely to undergo subsequent allo-HCT, our decision is generally favoring CD19CAR T-cell therapy over blinatumomab. This choice is influenced by long-term CAR T-cell persistence and durable remissions observed following CD19CAR T-cell therapy for advanced ALL, even without allo-HCT consolidation.14,17,22 In contrast, patients with r/r ALL (≥5% blasts) who achieve CR following blinatumomab typically relapse without allo-HCT consolidation. Blinatumomab in this setting is better used as a bridging therapy rather than a definitive curative treatment. We have shown that relapse is common in patients who did not receive transplants who responded to blinatumomab, with significantly lower 1-year EFS for patients who did not receive transplants compared with those who did (6% vs 56%).19 Tables 1 and 2 show the number of patients who received allo-HCT pre- and postblinatumomab and CD19CAR T-cell therapy in clinical studies.
Importantly, follow-ups remain short for current published studies, and the durability of remission post–CD19-targeted immunotherapies with or without allo-HCT can be influenced by several factors. For instance, success of CD19CAR T-cell therapy may be influenced by unique CAR product characteristics including the specific costimulatory signaling domain (ie, 4-1BB vs CD28)40 in the CAR construct. Other factors such as CD19CAR T-cell persistence, lymphodepleting regimen, disease burden at baseline, and MRD status posttreatment may also influence the durability of response to CD19CAR T-cell therapy.14,41
Long-term remissions were noted in the CHOP and multicenter tisagenlecleucel CAR studies using 4-1BB costimulation, despite the fact that most patients did not receive allo-HCT consolidation.17,22 Similarly, Park et al from MSKCC observed that allo-HCT consolidation did not affect long-term outcomes in patients who attained MRD− response post-CD19CAR T-cell therapy using CD28 costimulation.14 In contrast, the National Cancer Institute investigators reported high relapse rates post-CAR T-cell therapy using CD28 costimulation in patients who did not receive allo-HCT consolidation, compared with those who did (86% vs 10%; P = .0001).42 Likewise, Pan et al27 also reported high relapse rates among responders to CD19CAR T-cell therapy with 4-1BB costimulation who did not undergo allo-HCT consolidation, compared with those who did (60% vs 6%; P = .023). Thus, the role of allo-HCT consolidation following CD19CAR T-cell response currently remains a matter of debate, and until it is resolved we continue to recommend transplant to our eligible patients.
In this case, our rationale for selecting CD19CAR T-cell therapy was the fact that our patient had a late relapse (>1 year) post–allo-HCT, was no longer on immunosuppressive therapy, and had no recent history of GVHD, making autologous T-cell collection feasible. Furthermore, our choice was influenced by the fact that CD19CAR T cells have the potential to produce durable remissions in patients who may not be able to receive a second transplant.
Patient 4: the long wait for CAR T-cell manufacturing
Patient 4 was a 36-year-old man diagnosed with ALL with KMT2A gene rearrangement, who failed to respond to induction chemotherapy. He achieved MRD− CR with blinatumomab, followed by an allo-HCT from an MSD but relapsed 3 months later. His leukemia retained CD19 expression. He was enrolled on a CD19CAR T-cell clinical trial (NCT02146924), underwent leukapheresis, and received cytoreduction with liposomal vincristine. Five weeks later, he was admitted for lymphodepletion and CAR T-cell infusion, but had developed a fever and hyperbilirubinemia. He was diagnosed with liver GVHD and failed to respond to several lines of therapy. Eventually, patient 4 suffered septic shock and died without receiving his CD19CAR T cells.
Most studies using CD19CAR T-cell therapy use the patient’s autologous T cells to generate the final product. Thus, each patient must undergo leukapheresis and wait until the collected T cells are transduced with the CD19CAR, expanded to the therapeutic dose, and released for use, before they are ready for infusion. This process takes 4 to 6 weeks, which is challenging in advanced ALL, especially in cases with proliferative disease. Interim salvage therapy is often required to control ALL, which increases risk for serious toxicities that may eventually preclude the patient from receiving CD19CAR T cells, as with our unfortunate patient. Park et al from MSKCC reported 24 of 78 patients enrolled in their study who underwent leukapheresis yet did not receive CD19CAR T-cell infusion due to receiving alternate therapy, death during salvage treatment, infectious complications, or production failure.14 In the Novartis multicenter study, 17 of 92 patients were enrolled but subsequently excluded from the final product infusion due to toxicity or death.17 Table 2 highlights the number of patients in published CD19CAR T-cell studies who were leukapheresed but did not receive their cells. In contrast, blinatumomab is not a patient-specific product and is available immediately. Thus, blinatumomab is a better option for cases in which the patient cannot afford to wait for CD19CAR T-cell manufacturing. However, for a subset of patients with early or slowly relapsed ALL who can wait for T-cell manufacturing either without salvage therapy or with low-intensity therapy, CAR T cells are a reasonable option. Here, the goal of salvage therapy is to control the disease rather than to induce remission, and avoiding highly toxic salvage regimens that may result in the deterioration of the patient’s clinical status and their exclusion from receiving T cells is recommended.
Given concerns regarding the delay between enrollment and CAR T-cell treatment, efforts are ongoing to generate off-the-shelf allogeneic CD19CAR T cells. One such allogenic product is UCART19, which is derived from healthy donors by knocking out TRAC and CD52 genes to allow administration in non–HLA-matched patients. In a preliminary report of 20 patients, the CR/CRi rate was 88%, whereas severe CRS was observed in 15% and only 2 cases developed grade 1 skin GVHD.43 Other allogeneic CD19CAR T-cell products, including PBCAR0191 (NCT03666000), are being actively studied. Thus, off-the-shelf CD19CAR T-cell therapies may eventually allow rapid treatment of patients upon relapse of ALL.
In this case, we selected CD19CAR T cells given the higher expected response rate compared with retreatment with blinatumomab (36% based on limited data44 ), and the anticipation that CD19CAR T cells could provide durable remission in absence of a second transplant. However, this case highlights the challenge of using CAR T cells in early relapses post–allo-HCT, where GVHD flare upon discontinuing immunosuppressive therapy or development of significant toxicities during T-cell manufacturing could preclude T-cell infusion.
Patient 5: CD19 expression loss after relapse post–CD19-targeted immunotherapy
Patient 5 was a 46-year-old man diagnosed with ALL with t(4;11). He failed to respond to 2 cycles of induction. He was treated with blinatumomab and achieved MRD− CR, and then was referred to us for allo-HCT from an MSD, which he underwent without major complications. He relapsed 7 months later with CD19− ALL. Due to the CD19− status, he could not enroll in a CD19CAR T-cell study. He failed to respond to 2 other clinical studies and eventually died with progressive leukemia and infection.
When treating patients with advanced ALL, the goal is to deliver all available salvage therapies sequentially to prolong survival. However, with CD19-targeted immunotherapy, a subset of cases loses CD19 antigen expression at relapse. There are several distinct mechanisms of antigen loss in ALL following CD19-targeted immunotherapies, including clonal lineage switch to myeloid phenotype (common with KMT2A [MLL] rearrangement),45-50 outgrowth of CD19− leukemia clones existing at diagnosis,51 CD19 protein alterations by alternative mRNA splicing,52 and genetic mutations in exons 2 to 5 of the CD19 gene that promote protein truncation.53 Loss of CD19 by whatever mechanism precludes treatment with other CD19-targeted therapies, as seen for patient 5.
We previously reported that 35% of blinatumomab responders relapsed with CD19− ALL, whereas only 18% of blinatumomab-refractory patients lost CD19 expression at the time of progression.19 Longer follow-up from a phase 2 study of blinatumomab in MRD+ ALL found that 33% of relapses with available CD19 expression assessment were CD19−.54 In contrast, a multicenter study reported that only 8% of patients evaluated were CD19− at the time of progression.55
CD19 antigen loss has also been documented following CD19CAR T-cell therapy. The incidence of CD19− ALL post-CD19 CAR T-cell therapy varied in studies for relapsed cases, ranging from 16% to 100%.14,15,17,21,22,25 In the largest published multicenter study, 15 of 22 relapses (68%) post-CD19CAR T-cell therapy were CD19−.17 In contrast, the incidence of CD19− ALL relapse was only 39% in a Seattle Children’s Hospital study.21 Thus, more information is needed to determine how severely CD19CAR T-cell therapy affects CD19 loss at relapse of ALL. Tables 1 and 2 depict the rate of CD19− relapse following blinatumomab and CD19CAR T-cell therapy.
One way to combat the problem of CD19 antigen loss is targeting other molecules/antigens that might be more difficult to disrupt, or that could be combined with CD19. CD22 is another promising antigen target for ALL because it is also selectively expressed in B cells and has been effectively targeted with the antibody-drug conjugate, inotuzumab (CR/CRi in r/r ALL = 81%).56 In a study utilizing CD22-targeted CAR (CD22CAR) T-cell therapy for advanced ALL, which included patients who failed prior CD19-targeted immunotherapies, an encouraging CR rate (73%) was reported, including remission in all patients who had CD19− ALL at relapse.57 Unfortunately, this study also reported that 7 of 8 relapses post-CD22CAR T-cell therapy had diminished CD22 expression.57
Other promising ALL immunotherapeutic targets currently being explored include B-cell–activating factor receptor,58 CD12359 (NCT03739606), and thymic stromal lymphopoietin receptor.60,61 To avoid antigen loss, CAR T-cell therapies redirected toward 2 targets are being evaluated in the clinic, including dual (2 different antigen-specific CARs) and bispecific (1 CAR targeting 2 different antigens) (NCT03330691, NCT03125577, NCT03593109). Preclinical data suggest that dual CAR constructs can offset antigen escape in response to immunotherapy.60,62 Although this idea is provocative, clinical data have yet to prove that this approach is superior to sequential single-antigen targeting therapy.63,64
The majority of CD19CAR T-cell studies have allowed enrollment of patients with prior blinatumomab therapy, which does not appear to influence response to CD19CAR T cells as long as CD19 expression is preserved.14,15,22,41 In contrast, data on the activity of blinatumomab post-CD19CAR T-cell therapy are largely anecdotal.65 Although CAR T cells followed by blinatumomab is possible, it cannot be selected with high confidence.
In conclusion, treatment with blinatumomab and CD19CAR T cells holds promise in advanced ALL, allowing more patients to attain remission and possible cure with and without additional therapies. Both treatments have unique limitations and advantages, and the treating physician should be discerning when selecting treatment of each case. Table 3 summarizes considerations when choosing a CD19-targeted immunotherapy. Extensive research is ongoing to address the strengths and shortcomings for each CD19-targeted immunotherapy to expand their utilization and application in advanced ALL.
Acknowledgment
The authors thank Mary Clark for assistance in editing the manuscript.
Authorship
Contribution: I.A. and S.J.F. assembled the cases, analyzed the literature data, and wrote and approved the final manuscript.
Conflict-of-interest disclosure: S.J.F. has received licensed intellectual property and funding for clinical trials and continued laboratory studies from Mustang Bio. I.A. is on the advisory board with KITE Pharma and is a consultant to Autolus Limited.
Correspondence: Stephen J. Forman, Department of Hematology and Hematopoietic Cell Transplantation, City of Hope Medical Center, 1500 E. Duarte Rd, Duarte, CA 91010; e-mail: sforman@coh.org.