Introduction:
Hematopoietic stem cell transplantation (HSCT) has been widely employed for autoimmune disorders under myeloablative and non-myeloablative regimens. The main indication for HSCT in this setting is multiple sclerosis (MS) in its relapsing-remitting form and related disorders such as neuromyelitis optica or clinical isolated syndrome. Results have varied, but response rates and prognostic features are still unkown along the spectrum of disease and conditioning regimens.
Methods:
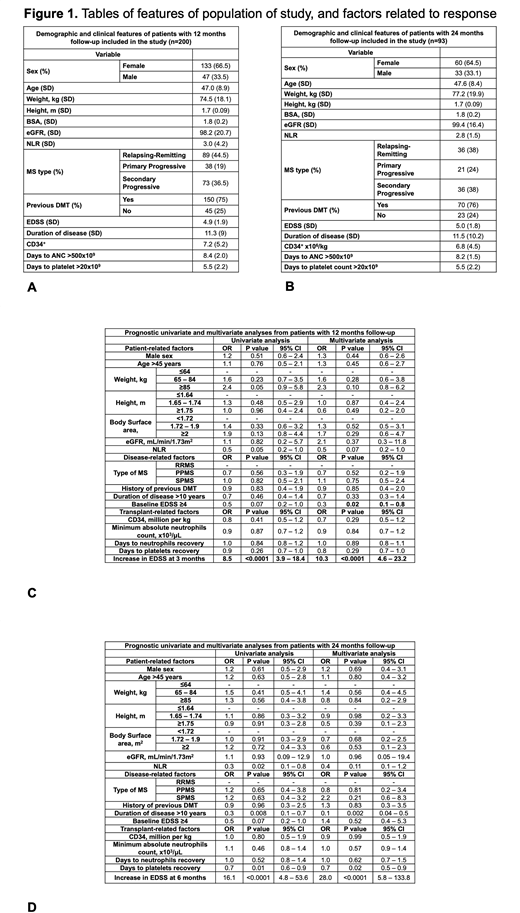
People with MS (PwMS) autografted from March 2015 to March 2020 with a reduced intensity regimen (Cy/G-CSF + Rituximab) (NCT 02674217), were followed longitudinally every 3 months to assess the Expandable Disease Status Scale (EDSS). All patients with complete follow-up data were included in this study and two different cohorts were made according to PwMS that were followed by 12 or 24 months. The primary outcome was improvement or stabilization of EDSS at 12 months and 24 months. All potential prognostic factors were collected from electronic medical record of patients with complete sociodemographic, clinical and laboratory data. In order to identify prognostic factors related to responses, univariate analyses were carried out with logistic regression; variables that showed a p value <0.15 were included in the multivariate analyses (using age, sex, type of MS, previous history of EDSS as covariates) with logistic regression. All patients signed a consent to authorize intervention and contact for follow-up and the protocol study was approved by the Institutional Ethics Committee.
Results:
Two cohorts were formed according to follow-up periods. Cohort 1 (12 months follow-up) comprised of 200 pwMS, 133 (66.5%) being female and 47 (33.5%) male. Their features are shown in Figure 1A. Cohort 2 (24 months follow-up) was formed by 93 pwMS, 60 (64.5%) being female and 33 (35.5%) male. Their features are shown in Figure 1B. In cohort 1, 149 pwMS (74.5%) had a response while 51 (25.5%) did not. Mean change of EDSS between baseline and 12 months post-HSCT was -0.42 (range -7 to 4). In cohort 2, 54 patients (58%) had a response while 39 (42%) did not. Mean change of EDSS between baseline and 24 months post-HSCT was -0.02 (range -4 to 7). In cohort 1, baseline EDSS ≥4 was identified as a predictor of 12 months response in multivariate analysis (OR 0.02, p 0.02, 95% CI 0.1- 0.8). Also, early response at 3 months post-HSCT in the univariate (OR 8.5, p <0.0001, 95% CI 3.9 - 18.4) and multivariate (OR 10.3, p <0.0001, 95% CI 4.6 - 23.2) analyses presented as a predictor of 12 months response. In cohort 2, early response at 6 months predicted response at 24 months post-HSCT in the univariate (OR 16.1, p <0.0001, 95% CI 4.8 - 53.6) and multivariate analysis (OR 28, p <0.0001, 95% CI 5.8 - 133.8). Furthermore, duration of disease >10 years showed an association with a negative response at 24 months as well in the univariate (OR 0.3, p 0.008, 95% CI 0.1 - 0.7) and multivariate analyses (OR 0.1, p 0.002, 95% CI 0.04 - 0.5). These results are shown in Figure 1C and 1D.
Conclusions:
Early response at 3 or 6 months may be robust measures that could translate in long term improvement or stabilization of disease. Although the effects showed in this study are profound and were replicated on two cohorts, these results should be interpreted with caution and a longer follow-up could confirm these findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.