INTRODUCTION: Pain, the most common complication of sickle cell disease (SCD), presents as both sudden acute pain and chronic daily pain. However, there is wide variability in frequency and presentation of pain despite inheritance of the same monogenic gene defect. SCD has long been recognized as a chronic inflammatory condition. The ongoing effect of repeated vaso-occlusion, ischemia-reperfusion injury and hemolysis contribute to further SCD inflammation and likely pain. Regulation of the immune response can potentially modulate the inflammatory impact on pain. The collective balance of these inflammatory mediators in union in SCD patients and how this balance may change during baseline health and acute pain is unknown. The objective of this work was to determine the balance between patients' inflammatory and immune regulatory response and examine whether this balance changes during acute pain in patients with SCD.
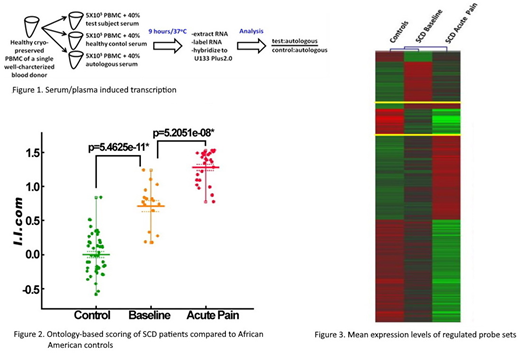
METHODS: We conducted a cross sectional analysis involving 3 cohorts: patients with SCD who were in their baseline health state, patients with SCD who had an acute pain episode and healthy African American controls. We used a novel bioassay originally developed for use in type 1 diabetes and applied to cystic fibrosis, inflammatory bowel disease and influenza to determine the inflammatory/immune regulatory response. This response was calculated as a composite Inflammatory Index (I.I.com) from these 3 patient cohorts. Patient plasma was co-cultured with cryopreserved PBMCs from a healthy donor to induce transcription (Figure 1). We identified informative transcripts that differentiate SCD patients from healthy controls thereby defining the disease-specific plasma-induced signature and retained ones differentially expressed between patients with SCD and controls that exhibit a fold change >1.4, ANOVA p-value of <0.05 and an FDR <10%. The data were subjected to ontological analyses for quantitative interpretation with Database for Annotation, Visualization and Integrated Discovery (DAVID) and Ingenuity Pathway Analysis (IPA). Our scoring strategy used the degree of induction of genes in inflammatory and regulatory ontological classes. The composite I.I.com was calculated using the average ratio between the mean log intensity of the genes classified as being "inflammatory" versus "regulatory". Independent samples Student's t-test was used to compare the mean I.I.com between 1) SCD baseline health cohort and controls and 2) SCD baseline health cohort and SCD acute pain cohort.
RESULTS: Plasma from 16 patients with SCD in baseline health, 27 patients with SCD with an acute pain episode, and 45 African American controls were collected and analyzed. The average age of the study population was 12.6 (SD=3.6) years old and 52.3% were female. Quantitative scoring of plasma-induced signatures showed SCD patients had significantly higher mean I.I.com during baseline health compared to controls (0.713 vs. -1.235-12, p=5.4625-11). In addition, patients with SCD during acute pain episodes had significantly higher I.I.com than patients in baseline health (1.282 vs. 0.713, p=5.2051-8) (Figure 2). Heat map in Figure 3 shows differential gene expression between the cohorts; green and red colors in heat maps represent lower or higher relative expression respectively.
CONCLUSION: Our findings show distinct immune signatures in SCD patients compared to controls and distinct signatures in SCD patients during acute pain episodes as compared to baseline health. The novel assay used to assess the inflammatory and immune regulatory gene expression in the three cohorts studied allowed for the determination of the balance between the two immune states. The imbalance between inflammation and immune regulation shown in our results in SCD patients of SCD pain. Further investigation into the specific inflammatory pathways that contribute to altered immune response could lead to novel targets for pain treatment.
Mucalo:NIH/NINDS: Research Funding; NIH/NHLBI: Research Funding. Jia:NIH/NHBLI: Research Funding; NIH/NINDS: Research Funding. Panepinto:NINDS: Research Funding; HRSA: Research Funding; NINDS: Research Funding; NHLBI: Research Funding. Roethle:NIH/NHLBI: Research Funding; NIH/NINDS: Research Funding. Hessner:NIH/NHLBI: Research Funding; NIH/NINDS: Research Funding. Brandow:NIH / NHLBI: Research Funding; Greater Milwaukee Foundation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.