Background: Frontline treatment of follicular lymphoma (FL) yields high response rates, but most patients relapse. In addition, response rates and duration of response have historically declined with subsequent treatments. These factors make management of this disease challenging. Therefore, this study was conducted to determine if an online, simulation-based continuing medical education (CME) intervention could improve clinical decision making of hematologists/oncologists (hem/oncs) regarding treatment selection for relapsed/refractory (R/R) FL.
Description of Intervention: A CME certified virtual patient simulation (VPS) was made available via a website dedicated to continuous professional development. The VPS consisted of 2 cases of R/R FL presented in a platform that allows hem/oncs to assess the patients and make diagnostic and therapeutic decisions supported by an extensive database of diagnostic and treatment possibilities, matching the scope and depth of actual practice. Case 1: Patient with FL who failed 2 prior lines of therapy (R-CHOP, bendamustine/obinutuzumab), past medical history (PMH) well controlled hypertension and poorly controlled type 2 diabetes, presenting with constitutional symptoms and needs 3rd line treatment. Case 2: Patient with FL who failed 2 prior lines of therapy (bendamustine/rituximab, lenalidomide/rituximab), PMH well controlled atrial fibrillation and ulcerative colitis, patient requests intravenous therapy because he has trouble remembering to take oral medications.
Methods: Clinical decisions were analyzed using a sophisticated decision engine, and tailored clinical guidance (CG) employing up-to-date evidence-base and faculty recommendations was provided after each decision. Decisions were collected post-CG and compared with each user's baseline (pre-CG) decisions using McNemar's test to determine p-values (P < .05 indicates significance). Data were collected between 11/20/19 and 2/19/20.
Results: At the time of assessment, 154 hem/oncs who made clinical decisions were included in the analysis. From pre- to post-CG in the VPS, hem/oncs were more likely to make evidence-based practice decisions in:
-Diagnosing patients with relapsed FL: 55% pre-CG and 73% post-CG (P < 0.001)
-Starting an appropriate treatment for a patient with R/R FL
----Case 1: Ordering idelalisib: 7% pre-CG and 33% post-CG (P < 0.001)
----Case 1: Ordering lenalidomide + rituximab: 6% pre-CG and 28% post-CG (P < 0.001)
----Case 1: Ordering duvelisib: 2% pre-CG and 9% post-CG (P < 0.001)
----Case 2: Ordering copanlisib: 32% pre-CG and 73% post-CG (P < 0.001)
The top rationales for selecting an appropriate treatment option were: recommended by guidelines, convenience of administration route, better efficacy compared to other agents, and best option based on patient comorbidities.
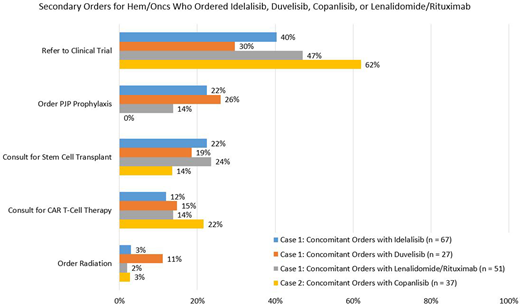
Other relevant concomitant therapies ordered were consult for chimeric antigen receptor (CAR) T-cell therapy, consult for stem cell transplant, radiation therapy, refer to a clinical trial, and Pneumocystis jirovecii pneumonia (PJP) prophylaxis (Figure 1).
Conclusion: This study demonstrates that VPS that immerses and engages hem/oncs in an authentic and practical learning experience improved evidence-based clinical decisions related to the management of R/R FL. This VPS increased the percentage of heme/oncs who correctly diagnosed R/R FL and selected an appropriate treatment option. This study indicates that unique educational methodologies and platforms, which are available on-demand, can be effective tools for promoting guideline-based therapy selection and clinical decision making.
Acknowledgement: This CME activity was supported by an independent educational grant from Bayer, Celgene Corporation, and Verastem Oncology. Jake Cohen contributed to data analysis for this research.
Reference: https://www.medscape.org/viewarticle/915986
Cohen:Janssen, Adicet, Astra Zeneca, Genentech, Aptitude Health, Cellectar, Kite/Gilead, Loxo: Consultancy; Genentech, BMS, Novartis, LAM, BioInvent, LRF, ASH, Astra Zeneca, Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract