Background
The MAVORIC study, a phase 3, open-label, multi-center, randomized controlled trial, compared the safety and efficacy of mogamulizumab with vorinostat in patients with mycosis fungoides (MF) or Sézary syndrome (SS) that relapsed/was refractory after ≥1 systemic therapy. Among patients treated with mogamulizumab, the confirmed global overall response rate (ORR; partial [PR] or complete response [CR]) was 28% (52/186), with a median duration of response of 14.1 months. The benefits of mogamulizumab treatment can be further characterized by assessing ORR and duration of response, both clinically important aspects of treatment success, together in a combined measure. For example, ORR4 describes a response lasting at least 4 months and was the primary endpoint in a phase 3 trial of brentuximab vedotin in patients with MF. The objective of this analysis was to assess the clinical and demographic characteristics of MAVORIC cohorts who have ORRs of different durations following treatment with mogamulizumab.
Methods
This post hoc analysis of MAVORIC, based on a secondary data analysis as of March 19, 2018, divided patients into 4 cohorts based on minimum duration of response (≥4, ≥6, ≥8, and ≥12 months; ORR4, 6, 8, and 12, respectively). Linear regression analysis (odds ratios [ORs] for ORR12 response) was performed for gender, baseline Eastern Cooperative Oncology Group (ECOG) Performance Status, disease type, disease stage (IB-IV), blood involvement, baseline CCR4 expression, age, time from diagnosis, mSWAT, and LDH. Stepwise multivariate analysis was carried out on the same factors. Blood samples at multiple time points after blood CR were collected from 2 SS patients in the ORR12 cohort at a single site, and the frequency of malignant TCR was monitored with the clonoSEQ next generation sequencing platform (Adaptive Biotechnologies; Weng 2013). Samples were assessed at baseline and every 3-6 months to monitor molecular minimal residual disease (MRD).
Results
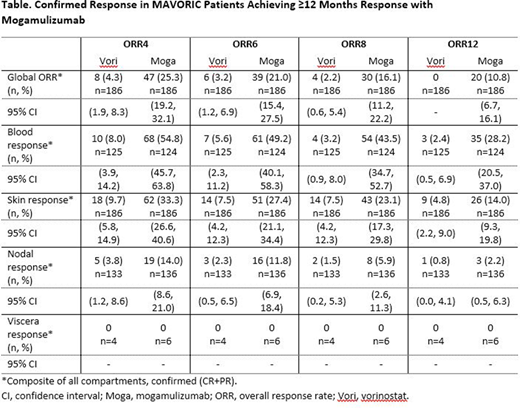
Response rates by disease compartment for patients treated for ≥12 months with vorinostat and mogamulizumab are shown in the Table. Among patients randomized to mogamulizumab (n=186), ORRs lasting ≥4, ≥6, ≥8, and ≥12 months were seen in 25.3%, 21.0%, 16.1%, and 10.8%, respectively. Responses in blood and skin lasting ≥6 months (ORR6) were seen in 49.2% and 27.4% of mogamulizumab-treated patients, respectively, compared with 5.6% and 7.5% of vorinostat-treated patients. When baseline characteristics of patients achieving ORR12 were compared with all other patients treated with mogamulizumab via linear regression analysis, ORR12 patients were more likely to have SS (P=0.016, OR 0.29), stage IVA1 disease (P=0.0002, OR 11.13), and any blood involvement (P=0.03, OR 0.19). There was no correlation between skin CCR4 level at baseline and likelihood of attaining ORR12. When ORR12 patients were compared with patients who achieved shorter responses (ie, ORR2 patients who did not reach ORR12), long-term responders were more likely to have stage IVA1 disease (P=0.006, OR 7.3). Stepwise multivariate analyses confirmed diagnosis of SS as a significant predictor of long-term response. In 2 patients in the ORR12 cohort from a single center (best response global CR), the molecular MRD was monitored after clinical clearance of blood Sézary cells by routine flow cytometry. A 71-year-old man with SS demonstrated CR in blood after 1 mogamulizumab cycle and in skin at cycle 3. At last follow-up, the frequency of malignant TCR sequence in blood remained barely detectable at <1 copy/million nucleated cells, confirming deep remission in blood lasting ≥47 months. A 77-year-old woman with SS also achieved blood CR at cycle 1 and skin CR at cycle 3. This patient discontinued mogamulizumab after 16 cycles due to hip replacement but maintained global CR at last follow-up with mostly non-detectable MRD (<1 copy/million nucleated cells) in blood 63 months from the first dose-50 months since discontinuing treatment.
Conclusions
Compared with patients with shorter responses, patients in the MAVORIC trial who achieved long-term (≥12 months) responses were those with SS (stage IVA1) or blood involvement. Available MRD analyses on ORR12 patients indicate the ability of mogamulizumab to produce lasting and deep responses in some patients.
Kim:miRagen: Research Funding; Merck: Research Funding; Neumedicine: Consultancy, Research Funding; Portola: Research Funding; Medivir: Membership on an entity's Board of Directors or advisory committees; Trillium: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Galderma: Membership on an entity's Board of Directors or advisory committees, Research Funding; Solingenix: Research Funding; Horizon Pharma: Consultancy, Research Funding; Kyowa-Kirin Pharma: Research Funding; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees; Innate Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Elorac: Research Funding; Forty Seven Inc: Research Funding; Eisai: Membership on an entity's Board of Directors or advisory committees, Research Funding; Corvus: Research Funding. Khodadoust:Kyowa Kirin: Consultancy; Seattle Genetics: Consultancy. de Masson:Kyowa Kirin: Research Funding. Ito:Kyowa Kirin Pharmaceutical Development, Inc.: Current Employment. Dwyer:Kyowa Kirin Pharmaceutical Development, Inc.: Current Employment. Herr:Kyowa Kirin, Inc.: Current Employment. Bagot:Kyowa Kirin: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees; Helsinn/Recordati: Membership on an entity's Board of Directors or advisory committees; Innate Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.