Background: AML is a clinically and molecularly heterogeneous disease associated with poor survival. Multiple disease-related factors including cytogenetic findings and gene mutations, as well as patient-related factors, such as demographics and African American (AA) heritage, have been identified that impact on pt outcomes. However, with recent improved survival it is unknown whether racial health disparities persist. Moreover, we are not aware of a large study that assessed possible race-associated molecular differences. Thus, the goals of our study were to 1) analyze the outcomes of adult AML pts in a nationwide population study, including possible impacts of sociodemographic, financial and racial disparities and 2) characterize molecular features of AA compared with those of Caucasian AML pts.
Methods: For a nationwide population analysis, the Surveillance Epidemiology End Results (SEER) Program of the National Cancer Institute was used to identify 11,190 adults aged 18-60 years (y) diagnosed with AML (excluding acute promyelocytic leukemia) between 1986 and 2015. To characterize molecular features we performed targeted sequencing of 81 genes in 1,339 AML pts treated on frontline Cancer and Leukemia Group B/Alliance for Clinical Trials in Oncology (Alliance) protocols based on standard intensity cytarabine/anthracycline induction followed by consolidation between 1986 and 2016. No Alliance pt received an allogeneic stem cell transplant in 1st complete remission (CR).
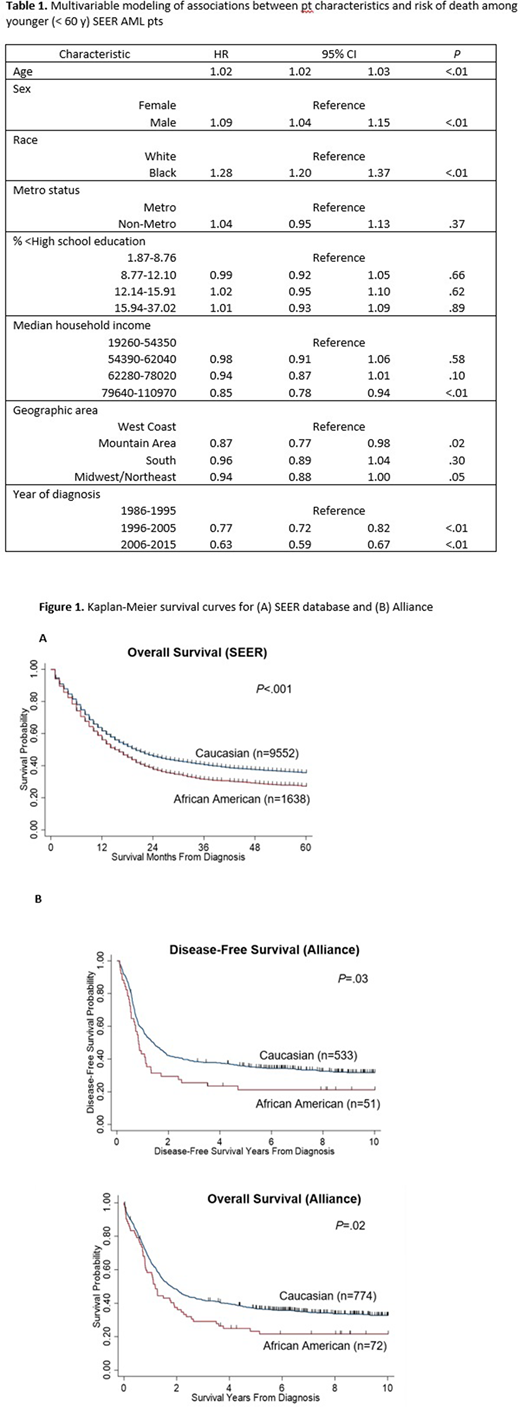
Results: The associations between demographic parameters and risk of death among SEER registry AML pts are shown in Table 1. While there was a slightly higher risk of death for men (HR 1.09) and a lower risk of death for pts with a higher median household income (>79.6k vs <54.4k, HR 0.85), the strongest factor affecting survival of AML pts was self-reported pt race, after accounting for other variables in the model. Specifically, AA AML pts had a higher risk of death compared with that of white AML pts (HR 1.28), with 3-year (y) overall survival (OS) rates of 32% and 41%, respectively (P<.001; Figure 1A). To evaluate if this race-associated survival disparity also persists in pts treated in the setting of clinical trials, we analyzed the survival of pts similarly treated on Alliance protocols. Although there was no difference in CR rates between AA and Caucasian Alliance AML pts, AA pts had inferior disease-free survival (DFS; median, 0.8 y vs 1.4 y, P=.02) and OS (median, 1.2 y vs 1.8 y, P=.02) compared with Caucasian pts, indicating that access to similar treatments might not alleviate racial survival disparities (Figure 1B). To assess whether any race-associated pretreatment features may help explain the different outcomes, we analyzed the clinical, cytogenetic and gene mutation features of the Alliance cohort. AA pts less often had normal cytogenetics (38% vs 51%, P=.01) and had a lower frequency of prognostically favorable NPM1 mutations (25% vs 38%, P=.04) and higher frequencies of spliceosome gene mutations (24% vs 12%; P=.009) than Caucasian pts. Multivariable analyses for outcome in AA pts did not identify any molecular features associated with achievement of CR or DFS. However, AA pts harboring FLT3-ITD or IDH2 mutations had shorter OS compared with wild-type pts (FLT3-ITD, HR=1.95, P=.03; IDH2, HR=2.17, P=.008). Notably, other well-established mutational features known to associate with outcome (e.g., NPM1 or TP53 mutations) did not impact on survival. Lastly, we performed uni- and multivariable outcome analyses for OS in our Alliance pts. Remarkably, being NPM1-mutated and not being AA were the only positive prognostic factors associated with longer OS in the final risk model (NPM1 mut vs wt, HR=0.72, P<.001; Caucasian vs AA, HR=0.72, P=.03).
Conclusion: Self-reported AA race is the most important pt-associated factor associated with poor survival in AML pts < 60 y of age based on SEER. Survival analyses in Alliance pts identify AA race as independent poor survival prognosticator in AML pts besides established molecular markers. . This disparity must be urgently addressed to ensure improved outcomes for AA AML pts, and larger studies to establish molecular risk profiles are needed.
Support: U10CA180821, U10CA180882 U24CA196171, https://acknowledgments.alliancefound.org; Clinicaltrials.gov Identifiers: NCT00048958, NCT00899223, NCT00900224
Bhatnagar:KaryoPharm Therapuetics: Research Funding; Cell Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees; Astellas: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; KITE: Membership on an entity's Board of Directors or advisory committees. Blachly:AbbVie, AstraZeneca, KITE Pharma: Consultancy. Mims:Novartis: Speakers Bureau; Jazz Pharmaceuticals: Other: Data Safety Monitoring Board; Syndax Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Kura Oncology: Membership on an entity's Board of Directors or advisory committees; Leukemia and Lymphoma Society: Other: Senior Medical Director for Beat AML Study; Agios: Consultancy. Walker:Vigeo Therapeutics: Consultancy; Karyopharm: Current Employment, Current equity holder in publicly-traded company. Powell:Genentech: Research Funding; Jazz Pharmaceuticals: Consultancy, Other: Advisor, Research Funding; Pfizer: Research Funding; Rafael Pharmaceuticals: Consultancy, Other: Advisor, Research Funding; Novartis: Research Funding. Kolitz:Magellan: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees. Stone:Biolinerx: Consultancy; Novartis: Consultancy, Research Funding; Celgene: Consultancy, Other; Aztra-Zeneca: Consultancy; Jazz: Consultancy; Argenix: Other; Janssen: Consultancy; Daiichi-Sankyo: Consultancy; Pfizer: Consultancy; Gemoab: Consultancy; Syndax: Consultancy, Research Funding; Takeda: Other: DSMB; Macrogenics: Consultancy; Trovagene: Consultancy; Syntrix: Other: DSMB; Abbvie: Consultancy, Research Funding; Agios: Consultancy, Research Funding; Actinium: Consultancy, Membership on an entity's Board of Directors or advisory committees; Astellas: Consultancy; Arog: Consultancy, Research Funding; Syros: Consultancy; Stemline: Consultancy. Byrd:Trillium: Research Funding; Leukemia and Lymphoma Society: Other; Acerta Pharma: Research Funding; Syndax: Research Funding; Pharmacyclics LLC, an AbbVie Company, Janssen, Novartis, Gilead, TG Therapeutics: Other; Janssen: Consultancy; Pharmacyclics LLC, an AbbVie Company, Gilead, TG Therapeutics, BeiGene: Research Funding; Pharmacyclics LLC, an AbbVie Company, Gilead, TG Therapeutics, Novartis, Janssen: Speakers Bureau; Kartos Therapeutics: Research Funding; Vincera: Research Funding; Novartis: Research Funding. Eisfeld:Karyopharm: Current Employment, Current equity holder in publicly-traded company; Vigeo Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.