Introduction
The earliest documented transmission of the coronavirus SARS-CoV-2, causing the disease Covid-19 occurred in the United Kingdom in February 2020. With data from Wuhan and Italy indicating a significant mortality rate in the region of 1-3% and identification of the risks of co-morbidities, hemato-oncology patients were quickly identified as being at a heightened risk from the virus due to baseline and chemotherapy induced immunosuppression. Data has shown that patients with cancer have a significantly higher incidence of severe events following infection with SARS-CoV-19 than those without cancer. Unlike many reported case series, our institution sees an unselected take of all hemato-oncology diagnoses within a large, ethnically-diverse locality and therefore provides an unfiltered snapshot of the impact of SARS-CoV-2 at an all-inclusive, population level.
Methods
Prospective data collection was carried out on all hemato-oncology patients admitted with a confirmed diagnosis of Covid-19 during March and April 2020 by reverse-transcriptase-polymerase-chain-reaction (RT-PCR) assay on a nasopharyngeal aspirate across two sites in one of London's largest District General Hospital Trusts. Our institution has a catchment area of 810 000 heads of population of which 38-46.5% are of black, Asian and minority ethnic (BAME) ethnicity depending on locality.
Results
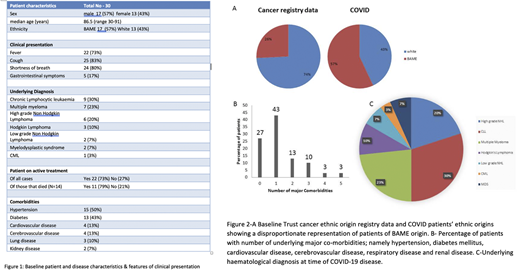
We identified a total of 30 hemato-oncology patients admitted with PCR proven SARS-CoV-19. Their baseline characteristics are shown in figure 1. When compared with our cancer registry data (Fig 2A) this highlights a disproportionate representation of BAME patients (57% of cases vs 26% of base population). Lymphoid malignancies and plasma cell dyscrasias (PCD) accounted for 90% of the admissions. CLL and PCD accounted for 30% and 23% respectively (Fig 2C).
Co-morbidities were less prevalent than those seen in patient cohorts without hematological malignancy. 70% of patients had </=1 co-morbidity and only 29% had >/= 2 comorbidities (Fig 2B) highlighting that, unlike other non-oncology series, hematological malignancy alone acts as a major risk factor for serious illness. Hypertension and Diabetes were the most common risk factors, seen in 50% and 43% of patients respectively.
The most common presenting features were cough (84%), fever (72%) and shortness of breath (80%). 16% had Gastrointestinal symptoms, but only seen in the context of concurrent respiratory symptoms. The vast majority (84%) had radiological changes consistent with a diagnosis of COVID-19.
Our cohort had a mortality rate of 47%. Of those that died, 57% were from BAME groups and 43% were White. 71% of those that died had either CLL (6/14 cases) or multiple myeloma (MM) (4/14 cases). CLL appears to be an independent risk factor from age, as two of the patients with CLL that died were amongst the youngest in our cohort (47 years and 59 years). Two patients that died had Myelodysplastic syndrome, one had Diffuse large B cell lymphoma and one had Hodgkin's lymphoma. We found that age and number of co-morbidities were positively associated with death. Of the patients that died, 79% were 70 years of age or over and the majority of survivors were 60 years old or younger (56%). Lymphopenia was a consistent finding at diagnosis (median lymphocyte count 0.8 x 109/l), neutropenia was rare (median neutrophil count 5.9 x 109/l) and C-reactive protein was elevated in all cases (median value 169, range 42-473 mg/l).
Of our 4 patients with plasma cell dyscrasias who died, 2 had end stage myeloma (4th line+ of therapy), 1 had primary refractory MM and 1 had plasma cell leukaemia, thus identifying these patients as extremely high risk from the outset.
Conclusion
It is of great importance to identify patient and disease specific risk factors conferring poor risk amongst our hemato-oncology patients. With shielding, invariably comes the increased risk of morbidity from social isolation and delayed presentation of non-COVID illness. Our data shows that CLL and BAME patients appear to be at particular risk of severe illness and poor outcomes. In a local ethnically diverse population, our patients are at heightened risk of morbidity and mortality and must be offered all strategies for interventions that may reduce likelihood of becoming infected with COVID 19 and should be considered early for vaccination, convalescent plasma and monoclonal antibodies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.