Background
Epstein-Barr virus (EBV) viremia - a condition of persistent active (vs latent) EBV infection - can be associated with a variety of life-threatening disorders. One such disorder is chronic active EBV (CAEBV), a type of primary immunodeficiency associated with high mortality rates. Another entity is EBV-driven (EBV+) hemophagocytic lymphohistiocytosis (HLH), characterized by a hyperactive immune response with elevated cytokines. Both can be associated with multi-organ dysfunction and failure. In addition, EBV viremia may be associated with complications following allogeneic hematopoietic cell transplantation (HCT) or can herald relapse of EBV+ malignancies. Tabelecleucel, an investigational off-the-shelf, allogeneic EBV-specific T-cell immunotherapy, has previously shown clinical activity in patients with EBV+ post-transplant lymphoproliferative disease (PTLD), EBV+ PTLD with central nervous system involvement and EBV+ leiomyosarcoma (Prockop S et al, JCI 2020; Kurlander et al, ESMO 2018) and is a potential therapy for CAEBV, HLH or EBVviremia in other life-threatening settings since it may control the EBV-based stimuli underlying these distinct diseases (Icheva V et al, J Clin Oncol 2013). Here, we report data in patients with complications of EBV viremia treated with tabelecleucel in an expanded access study (NCT02822495) within two non-overlapping protocols (EAP-201 [2016-2018] and EAP-901 [2018-present]).
Methods
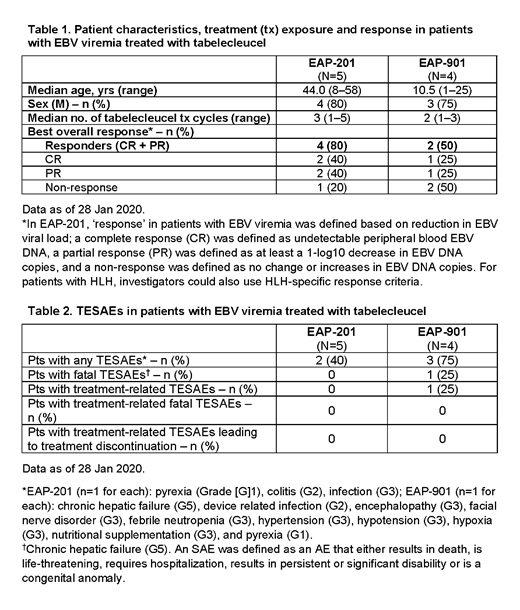
Eligible patients received tabelecleucel at ~2 x 106 cells/kg/dose on Days 1, 8 and 15, with laboratory assessments on Day ~28 of each 5-week cycle. EAP-201 enrolled patients with persistent EBV viremia (defined as serum EBV DNA assays showing detectable EBV viral load at least 4 weeks apart and known or suspected immunodeficiency or history of prior EBV+ malignancy) as well as patients with EBV+ HLH. EAP-901 includes patients with persistent EBV viremia and known or suspected immunodeficiency. Patients who did not respond could switch to tabelecleucel with a different human leukocyte antigen (HLA) restriction (restriction switch). In EAP-201, response criteria were based on reduction in EBV viral load and/or on HLH response criteria (Table 1). As EAP-901 is intended to provide compassionate access to tabelecleucel, limited patient data are collected compared with EAP-201; however, response is assessed by the investigators based on reduction in EBV viral load to determine whether an HLA restriction switch is needed. In both protocols, patients continued treatment until unacceptable toxicity, maximal response (2 consecutive complete responses [CR] or 3 partial responses [PR]), or up to 4 different HLA restrictions. Both protocols collected serious AEs (SAEs).
Results
Patient characteristics, treatment exposure, and responses are reported in Table 1; 5 patients with EBV viremia participated in EAP-201 and 4 in EAP-901. Objective response rates were 80% (n=4/5) for EAP-201 and 50% (n=2/4) for EAP-901. For EAP-201, the median time to first response for the 4 patients who responded was 1.7 (min 1.0, max 4.7) months, and for EAP-901 it was approximately 1 month for both patients who responded. Table 2 summarizes the treatment-emergent SAEs (TESAEs) observed with both protocols. EAP-901 reported a fatal SAE of chronic hepatic failure that was assessed as unrelated to treatment. One patient in EAP-901 experienced a grade 3 TESAE of facial nerve disorder that was assessed as possibly related to tabelecleucel; there were no other fatal or treatment-related TESAEs reported in either protocol, and no safety concern has emerged for this patient population.
Conclusions
Tabelecleucel was well tolerated and showed evidence of clinical activity in patients with life-threatening EBV viremia. Based on these results, further clinical investigation of tabelecleucel in patients with HLH or CAEBV is planned within an upcoming study (ATA129-EBV-205).
Ghobadi:Amgen: Consultancy, Research Funding. Stiff:CRISPR: Consultancy; Gamida-Cell: Research Funding; Atara Biotherapeutics: Research Funding; Amgen: Research Funding; Incyte: Research Funding; Takeda: Research Funding; Macrogenics: Research Funding; Eisai: Research Funding. Reshef:Kite: Consultancy, Research Funding; Atara Biotherapeutics: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy; Magenta: Consultancy; Incyte: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding; Pfizer: Consultancy; Celgene: Research Funding; Shire: Research Funding. Navarro:Atara Biotherapeutics: Current Employment, Current equity holder in publicly-traded company. Gamelin:Atara Biotherapeutics: Current Employment, Current equity holder in publicly-traded company. Dinavahi:Atara Biotherapeutics: Current Employment, Current equity holder in publicly-traded company. Sun:Atara Biotherapeutics: Current Employment, Current equity holder in publicly-traded company. Guzman-Becerra:Atara Biotherapeutics: Current Employment, Current equity holder in publicly-traded company. Prockop:Mesoblast: Consultancy, Research Funding; Atara Biotherapeutics: Research Funding; Jasper Pharmaceuticals: Research Funding; Memorial Sloan Kettering: Patents & Royalties: IP related to the development of third party viral specific T cells with all of my interests assigned to MSK.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract