Background: Myelodysplastic syndromes (MDS) are a group of clonal stem cell-derived disorders characterized by cytopenias, ineffective hemopoiesis, and a considerable risk of progression to acute myeloid leukemia (AML). Patients with MDS have higher rates of cardiovascular mortality, when compared to age-matched population. This has been attributed to the effects of chronic anemia, iron overload and systemic inflammatory state. Erythropoiesis-stimulating agents (ESA) have also been implicated. The aim of this study is to compare inpatient outcomes and readmissions in MDS patients admitted with congestive heart failure (CHF), to those without MDS.
Methods: Patients older than 65 years of age, with and without MDS, were queried for admissions of CHF between the years 2012 and 2017, from the Nationwide Inpatient Sample (NIS) database. T-test was used to compare means of continuous variables and chi-square test to compare proportions of categorical variables. Statistical tests for trends of resource utilization across six years were performed. Multivariable logistic regression was used evaluate risk factors for inpatient mortality. Then, we utilized the Nationwide Readmissions Database (NRD) to evaluate the readmission rates, as well as, the causes of readmissions among patients, with and without MDS, admitted with CHF during index admission, from 2016 to 2017.
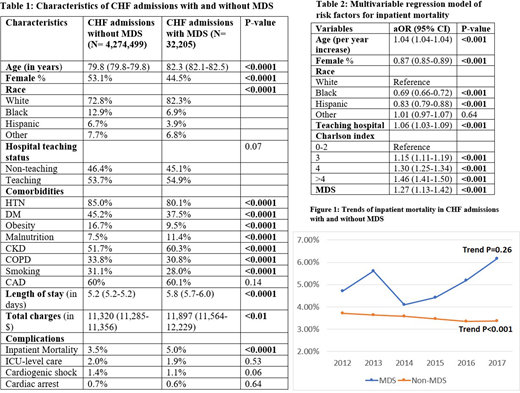
Results: A total of around 4.3 million admissions met the inclusion criteria, of which, 0.75% had MDS, accounting for 32,305 admissions. Mean age was higher in those with MDS (82.3 v 79.8 years, p<0.0001). Patients with MDS were more likely to be male (55.5% vs 46.9%, p<0.0001) and white (82.3% vs 72.8%, p<0.0001). There was a higher burden of comorbidities, including: hypertension, diabetes mellitus, obesity, smoking and obstructive lung disease in those without MDS, whereas chronic kidney disease was more common in the MDS group (p<0.0001 for all comorbidities).
Patients with MDS had higher inpatient mortality (5% vs 3.5%, p<0.0001), without significant differences in rates of cardiogenic shock, cardiac arrest, or need for intensive care. On multivariate analysis, after adjustment for age, gender, race, hospital teaching status and comorbidity burden, MDS was associated with higher risk of inpatient mortality (aOR 1.27 95% CI 1.13-1.42, p<0.001), longer length of hospital stay by 0.6 days (p<0.001) and higher hospitalization costs by $910 per admission (p<0.001).
There has been an increase in CHF admissions in MDS patients, from 7.96% in 2012 to 8.99% in 2017 (Trend p<0.001). While there was a statistically significant decrease in inpatient mortality in the non-MDS group (from 3.7% to 3.4%), there was a trend towards increased mortality in the MDS group, from 4.7% to 6.2%, although this did not reach statistical significance (p=0.26).
All-cause 30-day readmission rate was higher in those with MDS (27.7% vs 21.5%, p<0.0001). CHF accounted for a lower proportion of readmissions in the MDS group (31.9% vs 37.1%), whereas, infectious etiologies accounted for a higher share (13.9% vs 11.8%).
Conclusions: Therapy for MDS in the elderly is focused on improving quality of life, reducing deaths related to complications of cytopenias, or preventing progression to AML. Long-term survivors of MDS are more likely to suffer from cardiovascular disease, attributed to MDS itself or from complications of treatment. In our study, we have shown that MDS patients have higher mortality and resource utilization, as well as, higher rates of readmissions. In addition, hospitalization rates for CHF in MDS patients have been increasing. Some authors have advocated for addressing anemia early in the course of MDS to prevent downstream cardiac remodeling. Furthermore, attention to traditional cardiovascular disease risk factors in patients with MDS is imperative.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.