In this issue of Blood, Greiner and colleagues1 identify a high prevalence of hereditary α-tryptasemia (HαT) among patients with mastocytosis that is associated with an increased risk of severe mediator symptoms/hymenoptera venom anaphylaxis.
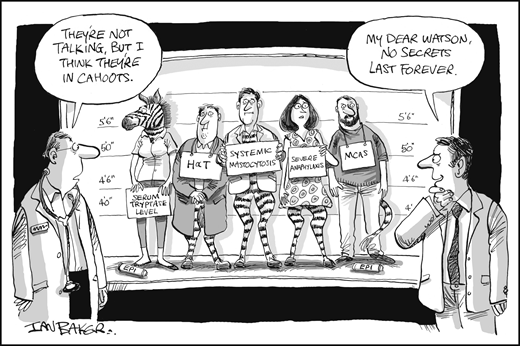
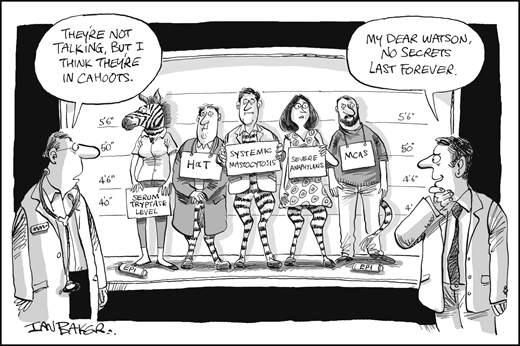
New evidence is shedding light on the relationship between HαT, clonal MC diseases, and severe mediator symptoms such as anaphylaxis. EPI, epinephrine. Professional illustration by Ian Baker; figure conceived by Jason Gotlib.
New evidence is shedding light on the relationship between HαT, clonal MC diseases, and severe mediator symptoms such as anaphylaxis. EPI, epinephrine. Professional illustration by Ian Baker; figure conceived by Jason Gotlib.
The diverse clinical presentations of systemic mastocytosis (SM) reflect neoplastic mast cell (MC)-related mediator release and organ damage. Although the latter signals advanced disease, symptoms of MC activation, such as flushing, diarrhea, and severe cardiovascular symptoms (eg, hypotension/anaphylaxis, hymenoptera venom allergy), occur across the spectrum of mastocytosis subtypes. Confusingly, and perhaps ironically, the most severe mediator symptoms are often found in patients with indolent SM, including some individuals with a very low percentage of bone marrow MCs. This discordance between the magnitude of symptoms and MC burden, and the well-known increased prevalence of anaphylaxis in mastocytosis, has led to several theories about the unusual, “twitchy” behavior of clonal, KIT D816V-driven MCs and their proclivity toward a lower threshold of degranulation. However, is it also possible that these aberrant MCs are the shiny object distracting attention from other, less obvious causes of a severe mediator phenotype?
The backstory to this inquiry relates to work by Jonathan Lyons and colleagues from the National Institute of Allergy and Infectious Diseases who sought to identify the biologic basis for, and clinical associations of, increased basal serum tryptase (BST) levels, which are found in ∼5% of the general population. In 2016, they identified single-allele extra copies of the TPSAB1 gene encoding α-tryptase as the basis for an autosomal dominant, multisystem disorder associated with elevated BST, which they termed HαT.2 The tryptase locus on chromosome 16 contains TPSAB1, which encodes either α- or β-tryptase isoforms, and TPSB2, which only encodes β-tryptase.
Affected individuals with HαT exhibit an array of symptoms, including cutaneous flushing, pruritis, chronic pain/arthralgias, and gastrointestinal dysmotility; dysautonomia and connective tissue abnormalities, such as joint hypermobility, are also common and may exhibit features overlapping with postural orthostatic tachycardia syndrome and Ehlers-Danlos syndrome type III. A gene dosage effect appears to be operative, with BST and symptom burden correlating with duplication, triplication, and even quintuplication of the TPSAB1gene.2,3 The initially studied cohorts showed no evidence of a clonal MC disorder, but exhibited elevated BST and some clinical features associated with MC activation, including spontaneous and provoked vibratory urticaria, and a two- to threefold increase in systemic venom reactions. These findings beg the question of whether some unique relationship exists between HαT and mastocytosis.
In short, the answer is “yes.” Greiner and colleagues’ study identified HαT in 17.2% of 180 mastocytosis patients, and only 4.4% of a control population that comprised sex-matched healthy controls and a large cohort of patients with myeloid neoplasms. Patients with HαT exhibited higher levels of BST compared with patients without HαT. The prevalence of HαT was enriched in patients with ISM and smoldering systemic mastocytosis (SSM) compared with cutaneous mastocytosis and advanced SM subtypes. A strong association of HαT with hymenoptera venom allergy as well as severe cardiovascular symptoms, such as hypotension and anaphylaxis, was found in mastocytosis patients.1 These findings are strikingly similar to recent results independently reported by Lyons and colleagues.4
With a specific epidemiologic association having now been established between an inherited disorder of increased TPSAB1 copy number and an acquired disease of clonal MCs, the next chapter for medical detectives is to unravel the biologic linkage between these diagnostic zebras (see figure). For example, it is unknown whether the number of germline copies of TPSAB1 conveys a genetic predisposition not only for HαT but also for later development of mastocytosis. Basic research investigations of how expression level of α-tryptase modulates MC homeostasis and neoplastic MC growth and the relevant autocrine or paracrine mechanisms that govern such interactions in the bone marrow microenvironment are sure to follow. Recent work has demonstrated that increased α-tryptase gene dosage favors the production of α/β-tryptase tetramers.5 In contrast to β-homotetramers, α/β-tetramers can activate protease-activated receptor-2 on a range of tissues, including endothelium, which may potentiate hypotension and anaphylaxis by increasing vascular permeability.5 It was also shown that α/β-tetramers make MCs more susceptible to vibration-triggered degranulation by cleaving the α subunit of the EGF-like module-containing mucin-like hormone receptor-like 2 mechanosensory receptor.5
The unexpected association between HαT and mastocytosis has several implications for routine practice and clinical trials. First, HαT appears to be a useful biomarker for symptomatic mastocytosis.1 TPSAB1 genotyping may help further inform patients about their risk of severe mediatory symptoms/anaphylaxis. Second, the presence of HαT raises questions about the validity of a BST level of 20 ng/ml as a minor diagnostic criterion for SM, especially with a concomitant diagnosis of HαT.6 Similar caveats may apply when using specific BST values to define SSM6 or to risk-stratify patients using prognostic scoring systems.7
A practical matter is how to sequence diagnostic testing. Should physicians prioritize screening for HαT in patients with a mildly elevated BST before performing a bone marrow biopsy to rule out SM? In patients with established HαT, is there a certain threshold of BST and/or symptom burden that provides a sufficient negative predictive value for SM such that a bone marrow biopsy can be deferred? With further challenges in interpreting BST introduced by HαT, should highly sensitive screening assays for KIT D816V,8 which can be performed on peripheral blood, carry more diagnostic sway? In light of such questions, diagnostic algorithms should be revisited and informed by outcome studies to identify best practices. Short of fulfilling a diagnosis of mastocytosis, HαT should also be considered in the differential diagnosis of MC activation syndrome (MCAS)9 presenting with a BST of ≥8 ng/mL, the minimum level observed in HαT.
In trials evaluating KIT-targeting therapies in SM, one of the challenges for response criteria will be how to interpret changes in BST levels and patient-reported symptoms because both are inexorably anchored to HαT and clonal MC burden. It is tempting to speculate about the value of incorporating a correction factor based on TPSAB1 copy number into therapeutic trials of SM to optimize adjudication of eligibility and response.
Irrespective of an accompanying diagnosis of mastocytosis, we are only beginning to understand what your HαT says about you. However, the multidisciplinary interest in these diseases should translate into rapid advances in clinical care. On the near horizon, antitryptase antibodies10 may offer the promise of mitigating severe mediator symptoms and life-threatening anaphylaxis.
Conflict-of-interest disclosure: The author served as chair of the study steering committee for the Novartis-sponsored global trial of midostaurin in advanced SM and chair or cochair of the study steering committees for trials of avapritinib and ripretinib in advanced SM. He has received funding to conduct trials of midostaurin, avapritinib, and ripretinib in SM. He has also served on advisory boards and received honoraria from Novartis, Blueprint Medicines, and Deciphera.