In this issue of Blood, Tarasco et al1 present, for the first time, prospective data collected from an international registry on the incidence and severity of acute thrombotic thrombocytopenic purpura (TTP) episodes in patients with hereditary/congenital TTP (cTTP). They also document the impact of prophylactic ADAMTS13 replacement therapy, the ADAMTS13 genotype, and patient age on these outcomes.
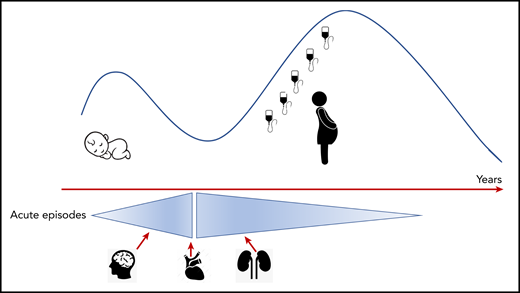
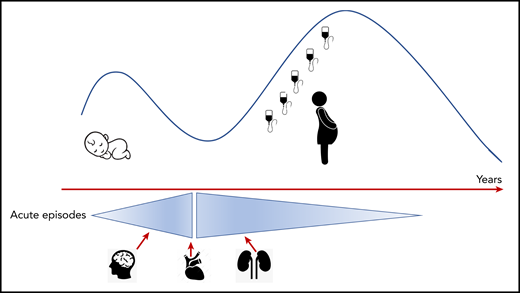
Presentation and acuity of congenital TTP. There is a bimodal distribution of presentation, in the neonatal period/early childhood and early adulthood, increased in women of child-bearing age. Acute TTP episodes are more common in children (<18 years) and organ involvement (brain, heart, and kidneys) with permanent end organ damage related to delayed cTTP diagnosis from presentation. The international registry does not document an increase in acute TTP episodes with age, but there does appear to be a higher risk of end organ damage when they occur.
Presentation and acuity of congenital TTP. There is a bimodal distribution of presentation, in the neonatal period/early childhood and early adulthood, increased in women of child-bearing age. Acute TTP episodes are more common in children (<18 years) and organ involvement (brain, heart, and kidneys) with permanent end organ damage related to delayed cTTP diagnosis from presentation. The international registry does not document an increase in acute TTP episodes with age, but there does appear to be a higher risk of end organ damage when they occur.
Hereditary TTP or cTTP was initially described by Schulman and colleagues in 1960.2 They presented a case of chronic thrombocytopenia in which plasma therapy resulted in an increase in the platelet count. In 1978, Upshaw3 concluded that his patient with recurrent acute episodes of severe thrombocytopenia had a congenital deficiency in a factor present in plasma that had an important role in red cells and platelets. For many decades, cTTP, an autosomal heterozygous inherited condition, was known as Upshaw-Shulman syndrome. The “deficient factor” was identified in the late 1990s; it was initially described as von Willebrand factor cleaving protease, and in 2001 it was defined as the metalloprotease ADAMTS13.4 Since identification of the ADAMTS13 gene, >150 mutations in cTTP have been reported. The case studies and series of patients with these mutations document varied presentations and clinical phenotypes.
The enzyme ADAMTS13 has a long half-life, initially reported as 3 days by Furlan and colleagues5 ; more recently it was revised to between 3 and 8 days. The half-life is impacted by individual rates of elimination, body weight, and basal metabolism.6 As a consequence, ADAMTS13 replacement, primarily with fresh frozen plasma, was projected to be required every 3 weeks. However, there is a paucity of clinical data on the clinical course of cTTP because of its rarity, with an estimated prevalence of 1 per million. In 2019, 2 “large” cohorts of cTTP patients were described, from the United Kingdom Thrombotic Thrombocytopenic Purpura Registry7 and from the International Hereditary Thrombotic Thrombocytopenic Purpura Registry.8 These findings set the scene for a better understanding of the condition and consideration for optimizing treatment. First, nonovert symptoms (ie, those symptoms present repeatedly in cTTP patients despite normal platelet counts) suggesting ongoing subacute microvascular thrombi were identified. The 3-week plasma infusion regimens were not adequate to eliminate these symptoms; reducing them to every 1 to 2 weeks was required. Second, prespacer domain mutations were associated with earlier onset of symptoms. Finally, prophylactic ADAMTS13 replacement reduced the incidence of end organ damage, such as stroke. The International Hereditary Thrombotic Thrombocytopenic Purpura Registry confirmed the bimodal presentation of cTTP (ie, in the neonatal period but more commonly in adulthood), and the presentation could not be predicted solely on the residual ADAMTS13 activity levels. The most striking finding from this registry was that 50% of the patients who were at least 40 years of age and were not on ADAMTS13 prophylaxis had ≥1 arterial thromboembolic event. Tarasco et al present further information on the annual incidence and severity of acute episodes of cTTP in patients receiving or not receiving regular prophylactic ADAMTS13 replacement.
The International Hereditary Thrombotic Thrombocytopenic Purpura Registry report on 87 patients included retrospective data and prospective follow-up. Neonatal hyperbilirubinemia was documented in 43%. Arterial events, including stroke, transient ischemic attacks, and myocardial infarction, were recorded in 36% of patients. One third of the cohort had renal disease, including 10% on dialysis, and 2 patients had received a renal transplant. Approximately 50% of patients were on regular ADAMTS13 prophylaxis therapy, one quarter were not receiving any treatment, and the remainder were on variable prophylaxis or data were lacking.
Not all children had acute episodes: 15 of 25 had recorded events and accounted for nearly half of all acute episodes in the entire cohort. However, the age at presentation of cTTP did not predict the frequency of acute episodes. Importantly, however, the time between overt disease and diagnosis of cTTP was associated with the highest prevalence of comorbidities, especially arterial events.
It was hypothesized that the frequency of acute episodes would increase with age, but these data suggest that the opposite is true. Indeed, the annual incidence of acute TTP episodes was 1.18 per year in patients younger than 10 years old, and it decreased with each decade. The primary precipitant of acute TTP episodes was acute infection (see figure).
The overall annual acute episodes risk was 0.35 per person per year and was not significantly different between patients who were and were not on prophylaxis. Seventy-nine percent of patients received fresh frozen plasma (10-15 mL/kg) every 2 weeks. Treatment with plasma infusion during an acute TTP episode took a median of 4 days, but it did not always resolve as promptly as expected (maximum, 43 days). To aid in the classification of the severity of acute episodes, a new scoring system was developed. The vast majority of acute episodes scored as 1. Scores of 3 were associated with significant comorbidities. Within the prospective period, 4 patients died (score = 4); 2 were in their third decade, and mortality was associated with severe cardiac and neurological disease.1
For ultrarare conditions, large registries provide important information that is critical to understanding demographics, symptoms, and the impact of therapy. Why is this important? As Tarasco et al describe, the use of plasma infusion is not adequate and carries considerable burden. So, what is the future? Recombinant ADAMTS13 for cTTP is in phase 3 clinical trials. It will have considerable advantages, including the ease of administration and the significantly higher ADAMTS13 activity levels achieved.9 How often should patients receive ADAMTS13 replacement? From the information regarding the risk of acute episodes and nonovert symptoms, weekly therapy seems preferable. The future looks hopeful for cTTP patients, but optimization and personalization of therapy will be critical.
Conflict-of-interest disclosure: M.S. has received funding for serving on advisory boards and speaker fees from Takeda, Sanofi, Alexion, Octapharma and Novartis and has received a research grant from Shire.