Abstract

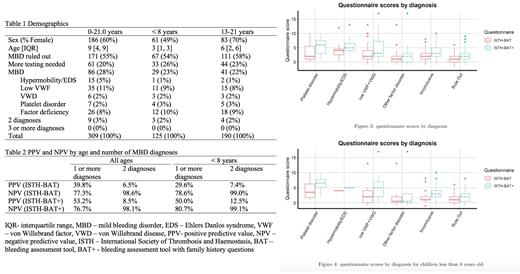
Bleeding assessment tools to standardize and interpret bleeding history have variable reported sensitivity and specificity to identify patients with mild bleeding disorders (MBD), particularly in subspecialty referral cohorts or younger patients with fewer hemostatic challenges. Here we review the predictive value of the International Society of Thrombosis and Haemostasis (ISTH) bleeding assessment tool, BAT, with or without the addition of 2 family history questions (FHQ), the BAT+, in our clinical cohort. Our hypothesis was that the addition of FHQ would improve the predictive value of the BAT for presence of a MBD in newly referred pediatric hematology clinic patients, particularly those < 8 yr. After 4 quality improvement cycles, a BAT flowsheet in the electronic medical record has been administered to new clinic patients referred to rule out MBD. The exploratory FHQ are added (BAT+), asking about the presence of a first degree relative with a bleeding disorder (yes = 1 point) or first- or second-degree relatives with any of a list of bleeding symptoms (yes = 1 point for each symptom). After IRB approval, electronic records from new clinic visits for "possible MBD" from 1/29/19 to 2/28/20 were retrospectively reviewed for clinical and demographic data, including scoring of the BAT/BAT+. Data are reported descriptively. Positive predictive values (PPV) and negative predictive values (NPV) were compared to assess the predictive power of dichotomized scores. The predictive power of continuous scores were assessed by comparing area under the curves (AUC) of receiver operating characteristics (ROC) curves for each questionnaire. To assess whether higher scores were predictive of multiple diagnoses, we estimated nested hurdle and Poisson regressions with robust standard errors, with the count of bleeding diagnoses as dependent variable and BAT/BAT+ scores as predictors. Over 13 months, in 313 new visits in patients ages 0-21 yr., 309 (98.7%) had BAT+ assessment and were evaluable. Common referral indications were abnormal lab results (48%), epistaxis (20%) and easy bruising (15%). Clinician-initiated documentation of screening for joint hypermobility by examination or history-taking occurred in 85 visits (28%), with 15 (5%) assigned a hypermobility diagnosis. At least 1 MBD was identified in 86 (28%) and 171 ( 55%) had MBD ruled out by the clinician. The average scores for BAT/BAT+ were 1.7/2.6 respectively for those judged by clinician not to have MBD, vs. 2.5/3.9 for 1 MBD diagnosis and 4/6.2 for 2 or more MBD. Using a threshold score of 3 for BAT as predictor of MBD in pediatrics, a threshold of 6 for the BAT+ was selected because its NPV for the whole group was close to that of the BAT for threshold of 3. For all patients and children <8 yr. the PPV of the BAT+ was higher than for the BAT, indicating better ability to predict MBD, for a comparable NPV. This was statistically significant (p=0.033) in the full sample and marginally so (p=0.064) among <8 yr. (Table 2). The AUC for the entire group were 0.597 (0.523-0.670) for the BAT, improving to 0.627 (0.555- 0.6) for the BAT+; however, for < 8 yr. the BAT AUC of 0.528 (0.396-0.660) vs. 0.559 (0.426-0.692) for BAT+ did not significantly differ. By Poisson regression analyses, higher scores on either the BAT or BAT+ predicted more diagnoses, with FHQ improving the goodness of fit (p=0.012) for the whole group (and similar but not statistically significant for < 8 yr.). Scores trended higher for platelet disorders and hypermobility than for low von Willebrand factor/disease or other factor deficiencies. We conclude that the BAT is helpful for standardizing bleeding history among clinicians and trainees and, with flowsheet format, can streamline documentation and sustain high utilization rates. While estimates suggest that FHQ improve predictive power of the BAT, a larger sample size is needed for confirmation. Threshold scores cutoffs based upon pubertal status and gender in < 21 year-olds may need to be lower than for older adults with additional hemostatic challenges. In the entire group and for <8 yr., the BAT under-performed compared to highest published estimates for PPV, NPV and AUC, as has been reported in recent, more rigorous literature, highlighting the complexity of evaluating young specialty referral populations for MBD.
Tarango: Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bayer: Membership on an entity's Board of Directors or advisory committees.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract